Two studies add to understanding of little-understood patient populations
Generalized epilepsy is surprisingly not uncommon among elderly patients with epilepsy, and older adults with drug-resistant epilepsy who cannot undergo surgery can safely be treated with responsive neurostimulation therapy (RNS). These two findings from separate Cleveland Clinic research investigations were presented at the recent 2021 American Academy of Neurology virtual annual meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The elderly is the fastest-growing population in this country, but most of what we know about epilepsy comes from managing children and younger adults,” says Cleveland Clinic epileptologist Vineet Punia, MD, MS, senior author of the two studies. “This research revealed some surprising findings and provides important information related to diagnosis and management in older and elderly patients.”
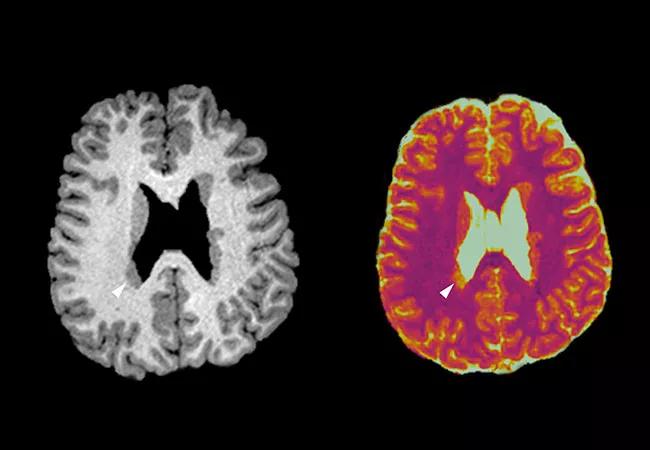
New-onset generalized epilepsy is most commonly seen in children, adolescents and young adults, in whom its clinical characteristics and management have been well described. Much less is known about its occurrence in the elderly, and generalized epilepsy has traditionally been thought to rarely develop as a new-onset seizure disorder in this age group.
This single-center cohort study offers the largest patient set of its type in the literature, with 30 patients at least 60 years old (mean age, 67.6; 63% female) who were admitted to a Cleveland Clinic epilepsy monitoring unit (EMU) and diagnosed with EEG-confirmed generalized epilepsy.
EMU evaluation was indicated to diagnose or characterize spells in 17 patients (56.7%) and to assess seizure burden in 13 others (43.3%). Key findings were as follows:
Advertisement
“We were surprised to find that a substantial proportion of elderly patients with generalized epilepsy developed it as an older adult,” says Dr. Punia. “It shows that we should not be too quick to always assume late-onset epilepsy is focal, and that further evaluation should be considered when indicated.”
Dr. Punia adds that his group is further studying generalized epilepsy in older and elderly patients outside of the EMU setting.
RNS has proven to be a safe and effective treatment for drug-resistant epilepsy in patients who cannot undergo surgery. However, RNS has not been specifically studied in older patients; investigations reported in the literature are with patients at an average age of about 35.
This retrospective study involved 57 patients treated at Cleveland Clinic with RNS for at least six months, including:
The cohorts had significant differences at baseline: the older group had more comorbidities (P < 0.01) and a longer duration of epilepsy (P < 0.01).
Results were as follows:
Advertisement
“Our findings show that RNS is a feasible and safe therapy for older patients with drug-resistant epilepsy who cannot undergo epilepsy surgery,” concludes Dr. Punia. “Outcomes in older patients compared favorably with those in younger patients despite the fact that the older patients tended to have longer duration of epilepsy.”
Dr. Punia notes that continued research in these age groups is important, as one should not assume that conclusions from studies on younger patients are universally applicable or that older and elderly patients have “grown accustomed to” their disorder and would not benefit from therapy changes. His group recently found that quality-of-life gains from epilepsy surgery reaped by older patients are similar to those in their younger counterparts.
Dr. Punia’s team is currently investigating how best to manage medications in older and elderly patients. “Some of these patients have been on the same medications for 50 years or more, and it’s worth taking a look at whether the medications are optimally effective with minimal side effects,” he adds.
Advertisement
Advertisement

Researchers explore the mental and physical benefits of social prescribing

Multidisciplinary approach helps address clinical and psychosocial challenges in geriatric care

Effective screening, advanced treatments can help preserve quality of life

Study suggests inconsistencies in the emergency department evaluation of geriatric patients

Auditory hallucinations lead to unusual diagnosis

How providers can help prevent and address this under-reported form of abuse

How providers can help older adults protect their assets and personal agency

Recognizing the subtle but destructive signs of psychological abuse in geriatric patients