Less morbidity seen with procedure for this population
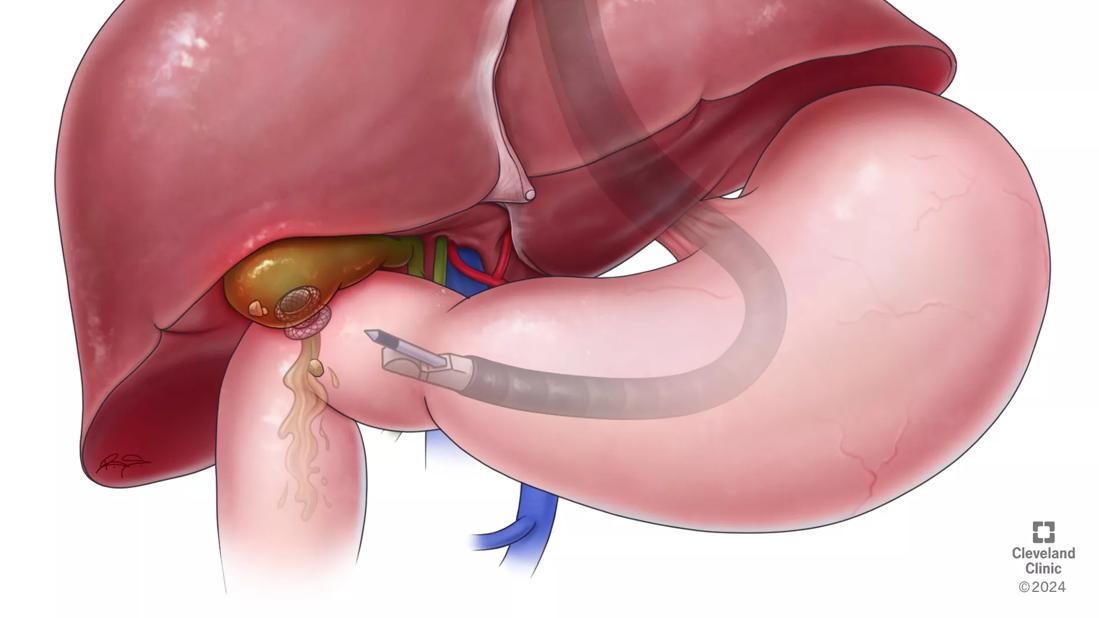
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b9551515-6634-48cb-976f-f5c7d1edaa45/EUS-Guided-Cholecystostomy-24-DDI-4816680)
cholecystostomy
Recently, a 75-year-old woman came to the emergency room due to unrelenting right upper quadrant pain, chills, nausea and vomiting. The patient had metastatic endometrial adenocarcinoma with peritoneal implants and was receiving chemotherapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient was evaluated by the gastroenterology and hepatology team and general surgery team at Cleveland Clinic. She was diagnosed with acute cholecystitis after physicians ordered a CT scan, a hepatobiliary iminodiacetic acid (HIDA) scan and magnetic resonance cholangiopancreatography (MRCP).
The optimal treatment was cholecystectomy. However, general surgery, interventional radiology, hepatology and gastroenterology experts consulted, they concluded that the patient was not a candidate for surgery due to her advanced cancer.
Nor was the patient a candidate for percutaneous cholecystostomy tube (PCT) placement by interventional radiology, a procedure in which a percutaneous catheter is placed in the gallbladder under imaging guidance. The catheter allows for drainage and decompression of bile from the inflamed gallbladder.
So the best option appeared to be endoscopic ultrasound (EUS)-guided cholecystogastrostomy, says Prabhleen Chahal, MD, an advanced endoscopist in the Digestive Disease & Surgery Institute.
“It’s potentially less morbid for patients who are unfit for surgery when compared to percutaneous cholecystostomy tube and usually takes 30 to 60 minutes of procedure time,” she says.“It can be performed transgastrically or transduodenally with placement of a covered or lumen-apposing metal stent. Multiple case series and multicenter data have shown comparable efficacy and fewer adverse events when compared with PCT.”
During the procedure, the patient was sedated and the endoscopic ultrasound was advanced through the mouth and esophagus then into the stomach and duodenum — allowing clear visualization and access of the gall bladder.
Advertisement
Then, using direct sonographic visualization, Dr. Chahal deployed a cautery enhanced lumen-apposing stent of 10 mm diameter that allowed for prompt decompression of the infected bile into the digestive tract.
Because the patient has widespread cancer, Dr. Chahal notes, there are no plans to remove the stent. Afterward, the patient’s pain resolved completely and she was discharged home the next day and was tolerating a regular diet.
Both PCT and endoscopic ultrasound-guided cholecystogastrostomy have risks including infection, perforation, bleeding, tube or stent malfunction. The latter, however has some advantages over PCT.
“Because the stent allows the endoscope to be advanced into the gall bladder for removal of stones prior to stent removal, it has a distinct advantage,” says Dr. Chahal, who is a leading expert in interventional EUS. “PCT is a mere drainage method and when the percutaneous tube is removed, the presence of stones in the gall bladder often leads to recurrent symptoms or infection.
“Furthermore, long-term presence of a drainage tube hanging from the abdomen can not only can interfere with quality of life, but can lead to issues like leakage and infection. The tube also needs to be replaced every four to eight weeks.”
Dr. Chahal says healthcare providers should offer this procedure as an alternative to percutaneous tube placement in patients with significant comorbidities such as cancer, severe heart, kidney or lung issues that precludes them from getting gall bladder surgery.
Advertisement
Yet, she adds, there is still a significant lack of awareness about EUS-guided drainage of gall bladder among both healthcare providers and patients.
“We need to spread the word about availability of this minimally invasive endoscopic procedure in high surgical risk patients,” she says.
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years