Director of the Pediatric Cardiac Catheterization Laboratory provides an overview of two new offerings
Following approval from the Food and Drug Administration (FDA), Cleveland Clinic Children’s is offering two cardiac catheterization options in the management of congenital heart conditions for select patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
TPV therapy is a nonsurgical modality in the treatment of chronic pulmonary regurgitation which frequently occurs as a result of previous surgical repair or percutaneous intervention in patients with tetralogy of Fallot, congenital pulmonary valve stenosis or a similar type of anatomy.
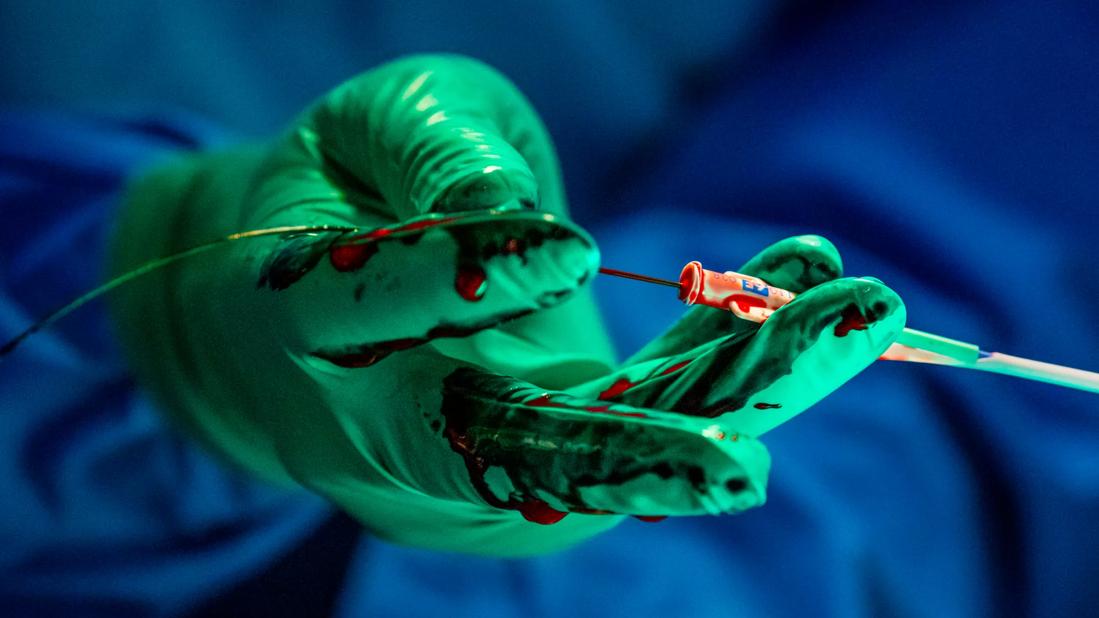
This percutaneous, nonsurgical approach delivers and deploys the replacement valve directly to the intended pulmonary valve site through a femoral or internal jugular veins. Once positioned in the right ventricular outflow tract, the valve, housed in a self-expanding stent, expands into place and begins working immediately. The Harmony™ TPV is the latest pulmonary valve approved for use in this particular indication in the U.S. by the FDA.
Up until the last decade, repair could only be achieved with open heart surgery. For patients, this might mean three to four days in the hospital, significantly more pain, and additional time at home recovering. Compare this with TPV, which takes about two to three hours to implant in the Cardiac Catheterization Laboratory. Patients generally spend about one night in the hospital and are prescribed a non-opioid analgesic regimen, explains Patcharapong Suntharos, MD, a pediatric and adult congenital interventional cardiologist and also Director of the Pediatric Cardiac Catheterization Laboratory at Cleveland Clinic.
“You have to remember, this patient population has, more likely than not, already had at least one open heart surgery and may have significant underlying comorbidities,” he says. “This option allows us to achieve the same outcome as a more invasive surgical approach but with the same, possibly better, outcomes.”
Advertisement
Since the device was approved in spring 2021, pediatric interventional cardiologists at Cleveland Clinic have completed several cases. So far the team has noted excellent outcomes with very few minor complications. Dr. Suntharos says, if all goes well, patients are seen in clinic following the procedure at one month, six months, one year, and then annually.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ba715603-d404-47d3-8325-3020fa4b8e91/CHP_3026203_06-08-22_075_LDJ_1-2-1024x699_jpg)
Patcharapong Suntharos, MD, Director of the Pediatric Cardiac Catheterization Laboratory at Cleveland Clinic.
Transcatheter occlusion isn’t a new technology; it’s become a choice option for many cardiologists in the repair of patent ductus arteriosus (PDA) in infants, children and adults. However, for extremely low birth weight infants, where the incidence of hemodynamic significant PDA is high, medical management or surgical ligation have been the only options — until recently.
The Amplatzer Piccolo™ Occluder is the first and only transcatheter treatment FDA approved in the treatment of PDA in premature infants with a birthweight as low as 700 grams.
The device, designed with a self-expanding nitinol mesh, is also delivered through a transcatheter system, guided from a small femoral vein only, without any femoral artery access, and guided into position with fluoroscopy and echocardiography, closing the PDA. Without arterial access, the risk of vascular injury in small, premature infants is extremely low.
Any NICU patient with a PDA significant enough that it requires closure is a candidate for the procedure, says Dr. Suntharos. He says the pediatric cardiology service works closely with Cleveland Clinic Children’s neonatologists to select good candidates for the intervention.
Advertisement
The procedure is generally completed in about an hour, and Dr. Suntharos says the babies wean off the ventilator faster than they would with a surgical procedure.
“In patients with the right indications, both techniques are minimally invasive options with good outcomes in an already fragile patient population,” he concludes.
Advertisement
Advertisement

Findings hold lessons for future pandemics

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes