Many approaches won’t delay therapy
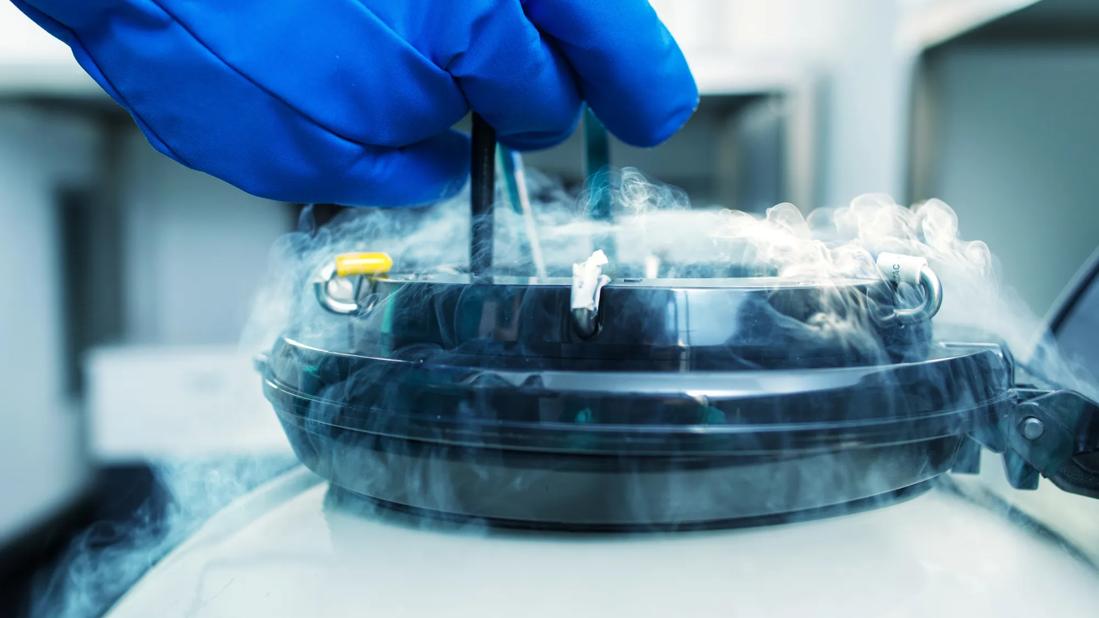
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a6a72a46-5165-4bf8-ba89-bbedb5b895ea/frozen-sperm-638504688)
Fertility freezing
Women with endometriosis, cancer, or other hematologic and autoimmune conditions, now have an array of ways to improve their ability to bear children following potentially gonadotoxic treatment. In fact, the chemo- and radiation therapies used to treat those conditions often damage the ovaries and cause a whole spectrum of symptoms that encompass delayed puberty, infertility and primary ovarian insufficiency, or menopause. Fertility preservation options should be discussed immediately upon diagnosis or soon thereafter with women of childbearing age or younger.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Robert DeBernardo, MD, Section Head of Gynecologic Oncology at Cleveland Clinic, and reproductive endocrinologist Laura Detti, MD, are part of a multidisciplinary team — including oncologists, Ob/Gyns fertility specialists, and minimally invasive surgeons— that is streamlining how Cleveland Clinic patients address the risk of treatment-induced infertility. The team’s goal is to move women faster through fertility preservation care (when desired) so therapeutic treatment isn’t delayed.
“As an oncologist, my primary focus is successful cancer treatment,” says Dr. DeBernardo. “But we’re seeing cancer in younger and younger women. Many of our cancer therapies can render women infertile or trigger early menopause. A thoughtful approach to fertility and hormonal preservation should be part of all cancer care for young women. In many cases, we still can have excellent oncologic outcomes without compromising fertility.”
The same is true for women with endometriosis, and hematologic and autoimmune conditions requiring chemotherapy, says Dr. Detti, Chair of Subspecialty Care for Women’s Health at Cleveland Clinic.
“Many factors determine the best fertility or hormonal preservation option for each patient,” she says. “It’s a case-by-case basis.”
Women with endometriosis have a 50% lower rate of pregnancy than women without endometriosis.
“If the ovary is occupied by an endometrioma, it will not produce healthy oocytes due to a decrease in ovarian follicles quantity and function,” says Dr. Detti. “Even if the patient doesn’t have endometriomas, she may have inflammation that causes a lower quality of eggs and abnormal endometrial maturation during menstrual cycles that impairs establishment of a pregnancy.”
Advertisement
Oocyte cryopreservation — which entails stimulation of ovarian follicles from which eggs can be harvested — and thus embryo cryopreservation may be difficult for women with large endometriomas. In those instances, Dr. Detti recommends ovarian cortex cryopreservation.
As of October 2019, ovarian cortex cryopreservation is no longer considered “experimental” by the American Society of Reproductive Medicine. The procedure requires removing and freezing a woman’s ovarian tissue, and then replanting the tissue later, after therapy is completed. Replanted ovarian tissue resumes natural hormone production.
“This fertility preservation technique is ideal for women having endometriosis surgery because ovarian tissue can be harvested during the same surgical procedure that removes endometriosis,” says Dr. Detti. “Following transplantation of the tissue, however, patients often need in vitro fertilization to conceive.”
Ovarian cortex cryopreservation also may be preferred for women with aggressive cancer who can’t delay therapy two to three weeks to go through the stimulation and surgical steps required for oocyte or embryo cryopreservation and it is the only option for the pediatric population, notes Dr. Detti. In fact, the ovaries of pre-pubertal girls cannot be successfully stimulated to allow for oocyte cryopreservation and this second option carries the advantage of restoring ovarian hormonal function after replant.
The Fertility Preservation multidisciplinary team at the Cleveland Clinic provides comprehensive counseling to identify the best option for each individual patient and offers all the currently available fertility preservation techniques. “No female, whether child, adolescent or adult, should see her fertility vanish because of chemo- or radiotherapy. Preservation of fertility can restore a quality of life similar to the one prior to treatments and our job is to make sure that everybody is included in the journey,” says Dr. Detti.
Advertisement
Ovarian cancer. “In younger women, we often can treat ovarian cancer successfully without needing to remove the uterus or the other ovary,” says Dr. DeBernardo. “The epithelial cancer of the ovary we more frequently see in younger women, known as borderline ovarian cancer, isn’t as aggressive and these patients can be managed conservatively. If we ultimately need to remove both ovaries, we can delay it until we harvest eggs or cryopreserve ovarian tissue so the patient can go on to have biological children.”
For borderline ovarian cancer, oocyte or embryo cryopreservation may be preferred instead of ovarian cortex preservation so the tumor isn’t inadvertently harvested with the ovarian tissue, notes Dr. Detti.
Cervical cancer. Most cases of cervical cancer are treated — and often cured — with pelvic radiation or radical surgery, making future pregnancy impossible. However, ovaries can be spared through ovarian transposition, a quick laparoscopic procedure that displaces ovaries outside the target radiation zone.
“We disconnect the ovary from the uterus and place it in the upper abdomen,” says Dr. DeBernardo. “It’s a relatively low-risk surgery, and the patient can begin pelvic radiation without delay.”
With healthy ovaries still producing viable eggs, women can use surrogacy to have their biological child. Even for women not planning to have children, ovarian transposition provides the benefit of natural hormone production.
Endometrial cancer. “About 10-20% of cases of endometrial cancer occur in premenopausal patients,” says Dr. DeBernardo. “Most of these cases are low grade and hormonally responsive. Patients can be treated successfully and go on to bear children. When they’re done having children, we can remove the uterus.”
Advertisement
Uterine transposition is an option for women preparing for pelvic radiation. The laparoscopic procedure moves the uterus, cervix and ovaries to the upper abdomen, away from the radiation area, while keeping them connected to the ovaries. Once pelvic radiation is completed, the patient has a second procedure to reposition the uterus and cervix at the top of the vagina. Because they haven’t been exposed to radiation, the uterus, cervix and ovaries function as normal.
Uterine transplantation, while not commonplace, also is a fertility-restoring option for women who were born without a uterus, or have had their uterus removed, notes Dr. DeBernardo.
“We need to educate more patients about the ability to preserve their fertility while effectively treating their cancer or other condition,” says Dr. DeBernardo. “There is a spectrum of care, and many options don’t require a delay in therapeutic treatment.”
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting