By Seth Rotz, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
*Please note: This is an abridged version of an article that originally appeared in the Cleveland Clinic Journal of Medicine. For the complete article please visit: https://www.ccjm.org/content/87/1/19.
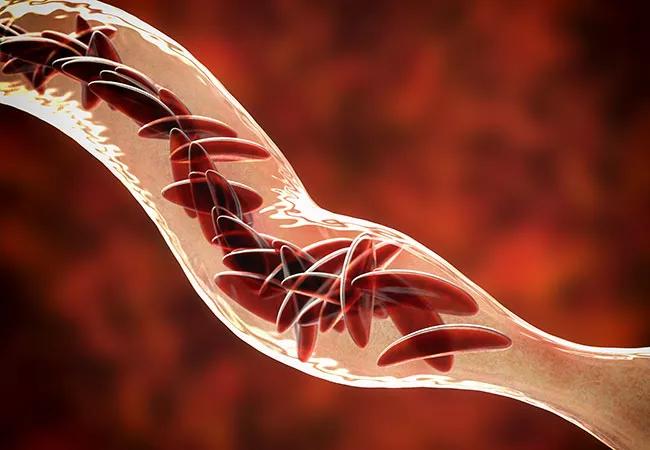
Approximately 100,000 people live with sickle cell disease (SCD) in the United States, and 1 of every 350 black children is born with the disease.1 Advances in health maintenance and therapy mean that more young patients are surviving to adulthood, requiring care in the adult primary care setting.
While the survival rate has improved for adults with SCD, their life expectancy is still more than two decades shorter than in the general population, as complications of chronic SCD interact with age-related non-SCD conditions and add to the disease morbidity.2–5 An alliance of patient, primary care physician, hematologist and other caregivers is crucial to optimizing disease outcomes, and the primary care physician is an important partner in providing optimal care of these patients. Here, we review mechanisms of sickle cell disease, common complications and their management based on current guidelines, and current approaches to health maintenance.
General management strategies
Current management strategies include prophylactic penicillin and immunizations to decrease the occurrence of pneumococcal infections, hydroxyurea (a disease-modifying agent), blood transfusions (for symptomatic acute anemia, stroke management, preoperative optimization) and bone marrow transplant.
In 2017, the US Food and Drug Administration (FDA) approved L-glutamine oral powder for reducing acute complications of SCD, and many other drugs are in development and undergoing clinical testing. Gene therapy is also progressing, with a recently reported successful outcome in one patient.7
The National Heart, Lung and Blood Institute (NHLBI) has developed guidelines for the care of SCD patients; the most recent version was published in 2014.8 The American Society of Hematology has developed new guidelines on the management of SCD complications, which are available here.
- The medical home model of care. Establishing a medical home—comprehensive care based on a partnership between the patient, family, primary care physician and other medical staff—is of paramount importance to the care of the SCD patient. Typically, care is provided by a hematologist in collaboration with the primary care physician. In some instances, a single setting is used, such as a comprehensive sickle cell clinic. Often, a primary care physician knowledgeable in the care of SCD functions as the sole provider. Referral to subspecialists is used as needed to manage disease complications.
- Regular medical evaluations. Regular medical evaluations are essential in assessing disease severity and progression. A detailed history and physical examination enable the clinician to note deviations from the previous clinical status and to identify new stressors. The regular visit is also an opportunity to address chronic complications, as discussed in the following sections. Efforts should be made to perform a yearly comprehensive review to screen for chronic complications of SCD and to facilitate specialty referrals.
- Immunization. Immunization status should be reviewed to ensure compliance with vaccinations.
- Albuminemia. Microalbuminemia screening is done through urinalysis and is confirmed with an albumincreatinine ratio. For micro- or macroalbuminuria with no other known cause, the NHLBI guidelines recommend angiotensin-converting enzyme (ACE) inhibitor therapy. Since the standard calculations of glomerular filtration rate cannot be used reliably in patients with SCD and in the acute setting, an increase in creatinine of 0.3 mg/dL should prompt an avoidance of nephrotoxic agents.
- Enuresis. Enuresis secondary to hyposthenuria (dilute urine) can occur, exacerbating dehydration. Adult patients may not wish to divulge this information voluntarily.
- Pulmonary hypertension. Pulmonary hypertension and acute chest syndrome are major causes of death in SCD. Guidelines for screening in SCD patients by the American College of Chest Physicians and the Pulmonary Hypertension Association recommend echocardiography or testing for plasma N-terminal pro-brain natriuretic peptide. However, the frequency of screening has not been established.26
- Osteopenia. Osteopenia with or without osteoporosis, defined by decreased bone mineral density, has been reported in up to 80% of adults with SCD. Significant vitamin D deficiency was associated with a higher prevalence of fracture history, secondary hyperparathyroidism and increased bone turnover.27 Studies have shown the potential benefit of vitamin D in reducing the number of pain days in SCD.27,28
- Avascular necrosis. Avascular necrosis can reduce the ability to perform activities of daily living. Though there is no standardized approach to prevention or therapy, early involvement of a physical therapist and orthopedic specialist can improve function and help assess the need for surgical intervention.
- Antibiotic prophylaxis. It has been recommended that patients with SCD who have a history of splenectomy or an invasive pneumococcal infection be placed on indefinite prophylaxis with penicillin.8
- Chronic pain syndrome. Chronic pain syndrome is described as pain that persists for at least three months. It is usually described as pain that is deep, nagging, achy and constant.29 Neuropathic pain resulting from peripheral or central nervous system dysfunction manifests as allodynia and hyperalgesia.29 Opioids are the mainstay of SCD pain management and may be used in conjunction with nonpharmacologic interventions. Clinicians need to be wary of stigmatizing these patients as drug-seekers, as this can result in delayed treatment and undertreatment. A doctor-patient relationship based on respect and trust will optimize pain management in these patients, and establishing this type of relationship should be a priority, as well as more frequent monitoring of disease status. While detailed management of chronic pain and pain crises in SCD is beyond the scope of this article, it should be noted that individualized pain management plans crafted with the participation of the patient or caregiver may help facilitate adherence. Concerns about drug-seeking behavior should be addressed after treatment of acute episodes. Effects of chronic opioid use (tolerance, dependence, and addiction) occur, and the provider may need to involve a pain management expert for collaboration in patient care.
- Neurocognitive effects of sickle cell disease. Neurocognitive dysfunction should be assessed with a focused history (memory deficits, work/school challenges, difficulties with medication adherence), followed by neuropsychiatric evaluation as appropriate. Vichinsky et al30 reported that adult patients with SCD who did not have neurologic symptoms remained at risk for neurocognitive performance deficits; their anemia may induce neurocognitive impairment secondary to cerebral hypoxemia undetected on standard neuroimaging. Early identification of patients with difficulties on specific measures of neurocognitive function may encourage earlier enrollment in cognitive rehabilitation programs.30
- Reproductive health. The regular evaluation should include discussion of fertility, contraception, erectile dysfunction and available treatment options. Before conception, genetic counseling should be offered to address modes of disease inheritance and transmission, as well as options for preimplantation genetic diagnosis. Pregnancy in SCD patients is a high-risk condition and warrants care from a team of specialists including a perinatologist, adult hematologist and specialists involved in the management of SCD-related complications.
- Medication adherence. Adherence to medications is a major challenge for patients with SCD. It can be improved during clinic visits by reviewing missed doses and providing tools to aid daily compliance, such as smartphone medication apps, pillboxes and calendar reminders. Patients with SCD undergo repeated interventions that require intravenous access (laboratory analysis, fluid resuscitation, transfusions), and over time, peripheral venous access becomes difficult.31 Central venous access is often required, and it is important to educate the patient about the proper care of these devices and potential complications such as thrombosis and infection.
- Psychosocial support. Patients with chronic illness face psychosocial stressors, and access to psychosocial support (psychologist, counselor, social worker) is of paramount importance in sustaining effective health maintenance strategies. Assistance can be provided for acquiring health insurance and transportation, joining support groups, and addressing educational and vocational goals.
Take-home messages
- With new advances, health maintenance and curative therapies are available.
- A team approach including the patient, caregivers, primary care physician and hematologists is crucial to optimizing disease outcomes.
- The primary care physician is an important partner in providing optimal care to adults with SCD.
References
- Ware RE, de Montalembert M, Tshilolo L, Abboud MR. Sickle cell disease. Lancet. 2017;390(10091):311–323.
- Thein SL, Howard J. How I treat the older adult with sickle cell disease. Blood. 2018;132(17):1750–1760.
- Serjeant GR, Chin N, Asnani MR, et al. Causes of death and early life determinants of survival in homozygous sickle cell disease: the Jamaican cohort study from birth. PLoS One. 2018;13(3):e0192710.
- Gardner K, Douiri A, Drasar E, et al. Survival in adults with sickle cell disease in a high-income setting. Blood. 2016;128(10):1436–1438.
- Elmariah H, Garrett ME, De Castro LM, et al. Factors associated with survival in a contemporary adult sickle cell disease cohort. Am J Hematol. 2014;89(5):530–535.
- Bunn HF. Pathogenesis and treatment of sickle cell disease. N Engl J Med. 1997;337(11):762–769.
- Ribeil JA, Hacein-Bey-Abina S, Payen E, et al. Gene therapy in a patient with sickle cell disease. N Engl J Med. 2017; 376(9):848–855.
- Yawn BP, Buchanan GR, Afenyi-Annan AN, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. 2014; 312(10):1033–1048.
- Serjeant GR. The natural history of sickle cell disease. Cold Spring Harb Perspect Med. 2013;3(10):a011783.
- Parent F, Bachir D, Inamo J, et al. A hemodynamic study of pulmonary hypertension in sickle cell disease. N Engl J Med. 2011;365(1):44–53.
- Blake K, Lima J. Asthma in sickle cell disease: implications for treatment. Anemia. 2011;2011:740235.
- Solomou E, Kraniotis P, Kourakli A, Petsas T. Extent of silent cerebral infarcts in adult sickle-cell disease patients on magnetic resonance imaging: is there a correlation with the clinical severity of disease? Hematol Rep. 2013;5(1):8–12.
- DeBaun MR, Armstrong FD, McKinstry RC, Ware RE, Vichinsky E, Kirkham FJ. Silent cerebral infarcts: a review on a prevalent and progressive cause of neurologic injury in sickle cell anemia. Blood. 2012;119(20):4587–4596.
- Menaa F, Khan BA, Uzair B, Menaa A. Sickle cell retinopathy: improving care with a multidisciplinary approach. J Multidiscip Healthc. 2017;10:335–346.
- de Melo MB. An eye on sickle cell retinopathy. Rev Bras Hematol Hemoter. 2014;36(5):319–321.
- Minniti CP, Eckman J, Sebastiani P, Steinberg MH, Ballas SK. Leg ulcers in sickle cell disease. Am J Hematol. 2010;85(10):831–833.
- Serjeant GR, Serjeant BE, Mohan JS, Clare A. Leg ulceration in sickle cell disease: medieval medicine in a modern world. Hematol Oncol Clin North Am. 2005;19(5):943–956.
- Naik RP, Streiff MB, Lanzkron S. Sickle cell disease and venous thromboembolism: what the anticoagulation expert needs to know. J Thromb Thrombolysis. 2013; 35(3):352–358.
- Naik RP, Streiff MB, Haywood C Jr, Nelson JA, Lanzkron S. Venous thromboembolism in adults with sickle cell disease: a serious and under-recognized complication. Am J Med. 2013;126(5):443–449.
- Novelli EM, Huynh C, Gladwin MT, Moore CG, Ragni MV. Pulmonary embolism in sickle cell disease: a case-control study. J Thromb Haemost. 2012;10(5):760–766.
- de Montalembert M, Deneux-Tharaux C. Pregnancy in sickle cell disease is at very high risk. Blood. 2015;125(21):3216–3217.
- Howard J, Oteng-Ntim E. The obstetric management of sickle cell disease. Best Pract Res Clin Obstet Gynaecol. 2012;26(1):25–36.
- Oteng-Ntim E, Meeks D, Seed PT, et al. Adverse maternal and perinatal outcomes in pregnant women with sickle cell disease: systematic review and meta-analysis. Blood. 2015; 125(21):3316–3325.
- AlDallal SM, AlDallal NM. Infertility issues in men with sickle cell disease. Int J Pregn & Chi Birth. 2017;2(3):88–90.
- Olambiwonnu NO, Penny R, Frasier SD. Sexual maturation in subjects with sickle cell anemia: studies of serum gonadotropin concentration, height, weight, and skeletal age. J Pediatr. 1975;87(3):459–464.
- Willen SM, Gladwin MT. What is the role of screening for pulmonary hypertension in adults and children with sickle cell disease? Hematology Am Soc Hematol Educ Program. 2017;2017(1):431–434.
- Osunkwo I, Ziegler TR, Alvarez J, et al. High dose vitamin D therapy for chronic pain in children and adolescents with sickle cell disease: results of a randomized double blind pilot study. Br J Haematol. 2012;159(2):211–215.
- Boettger PC, Knupp CL, Liles DK, Walker K. Vitamin D deficiency in adult sickle cell patients. J Natl Med Assoc. 2017;109(1):36–43.
- Ballas SK. Update on pain management in sickle cell disease. Hemoglobin. 2011;35(5–6):520–529.
- Vichinsky EP, Neumayr LD, Gold JI, et al; Neuropsychological Dysfunction and Neuroimaging Adult Sickle Cell Anemia Study Group. Neuropsychological dysfunction and neuroimaging abnormalities in neurologically intact adults with sickle cell anemia. JAMA. 2010;303(18):1823–1831.
- Shah N, Landi D, Shah R, Rothman J, De Castro LM, Thornburg CD. Complications of implantable venous access devices in patients with sickle cell disease. Am J Hematol. 2012;87(2):224–226.
- Niihara Y, Miller ST, Kanter J, et al; Investigators of the Phase 3 Trial of l-Glutamine in Sickle Cell Disease. A phase 3 trial of lglutamine in sickle cell disease. N Engl J Med. 2018;379(3):226–235.
- Jagadeeswaran R, Rivers A. Evolving treatment paradigms in sickle cell disease. Hematology Am Soc Hematol Educ Program. 2017;2017(1):440–446.
- Telen MJ. Beyond hydroxyurea: new and old drugs in the pipeline for sickle cell disease. Blood. 2016;127(7):810–819.
- Ataga KI, Kutlar A, Kanter J. Crizanlizumab for the prevention of pain crises in sickle cell disease. N Engl J Med. 2017;376(5):429–439.
- Estepp JH. Voxelotor (GBT440), a first-in-class hemoglobin oxygen affinity modulator, has promising and reassuring preclinical and clinical data. Am J Hematol. 2018;93(3):326–329.
- Johnson FL, Look AT, Gockerman J, Ruggiero MR, Dalla-Pozza L, Billings FT 3rd. Bone-marrow transplantation in a patient with sickle-cell anemia. N Engl J Med. 1984;311(12):780–783.
- Gluckman E, Cappelli B, Bernaudin F, et al; Eurocord, the Pediatric Working Party of the European Society for Blood and Marrow Transplantation, and the Center for International Blood and Marrow Transplant Research. Sickle cell disease: an international survey of results of HLA-identical sibling hematopoietic stem cell transplantation. Blood. 2017;129(11):1548–1556.
- Mentzer WC, Heller S, Pearle PR, Hackney E, Vichinsky E. Availability of related donors for bone marrow transplantation in sickle cell anemia. Am J Pediatr Hematol Oncol. 1994;16(1):27–29.
- Shenoy S, Eapen M, Panepinto JA, et al. A trial of unrelated donor marrow transplantation for children with severe sickle cell disease. Blood. 2016;128(21):2561–2567.
- Kodish E, Lantos J, Stocking C, Singer PA, Siegler M, Johnson FL. Bone marrow transplantation for sickle cell disease. A study of parents’ decisions. N Engl J Med. 1991;325(19):1349–1353.
- Bolaños-Meade J, Fuchs EJ, Luznik L, et al. HLA-haploidentical bone marrow transplantation with post-transplant cyclophosphamide expands the donor pool for patients with sickle cell disease. Blood. 2012;120(22):4285–4291.
- Ye L, Wang J, Tan Y, et al. Genome editing using CRISPR-Cas9 to create the HPFH genotype in HSPCs: an approach for treating sickle cell disease and beta-thalassemia. Proc Natl Acad Sci USA. 2016;113(38):10661–10665.