Developing noninvasive screening methods to assess embryo viability and encourage elective single-embryo transfer
Just 25 years ago, only one in 10 women undergoing fertility treatment went home with a baby. To be successful, a woman needed to accept the transfer of three or four embryos to her uterus, despite the increased risk of multiple pregnancy and associated neonatal and maternal complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Moreover, embryos were introduced in to the uterus at the two- to eight-cell stage. The single most important criteria for embryo selection was simply morphology at transfer, explains Nina Desai PhD, HCLD, who heads Cleveland Clinic’s IVF laboratory, located at Cleveland Clinic Beachwood.
Advances in clinical and laboratory protocols have since changed the overall landscape of IVF, with higher live birth rates and fewer embryos being transferred. And yet morphology has remained the predominant embryo selection criterion.
“In the last five years, two new technologies, namely time-lapse imaging and preimplantation genetic screening (PGS) have been adapted by clinics to get beyond ‘looks’ in embryo selection for transfer,” says Dr. Desai.
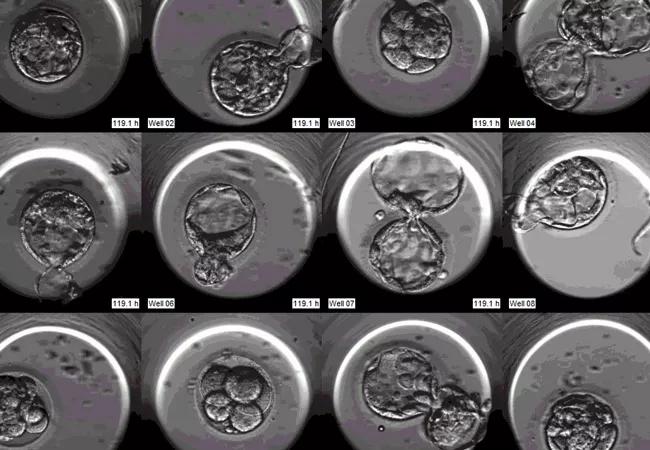
Cleveland Clinic introduced time-lapse imaging into its fertility practice in 2012. By 2014, all patients had the advantage of continuous undisturbed culture in the EmbryoScope, a meticulously engineered incubation chamber with sophisticated video capabilities for time-lapse imaging of embryos as they grow.
“The wealth of information from this technology has allowed the assessment of embryo implantation potential using cell-cycle kinetics and visualization of nuclear and cleavage anomalies,” Dr. Desai explains. “We routinely use this technology to identify high-potential embryos and transfer them singly to patients, ultimately helping achieve a healthy outcome for mother and child.”
Embryonic aneuploidy contributes significantly to failed implantation. PGS addresses this issue by selecting embryos based on chromosome status rather than morphology.
Advertisement
“This represents a significant shift in IVF practice, and most importantly, allows patients to elect to transfer a single euploid embryo with a high expectation of a positive outcome,” Dr. Desai says. “Pregnancy rates with transfer of a single euploid blastocyst range from 55 to 65 percent in our IVF program.” She notes, however, that PGS is quite expensive and very labor intensive and invasive, requiring excision of cells from the blastocyst using a laser.
A new study from the Cleveland Clinic IVF laboratory looks at the correlation between embryo growth kinetics and chromosome status with an eye toward finding a less invasive method to select euploid embryos.
“Preliminary data do indeed indicate that morphokinetic data available from time-lapse imaging may enhance the likelihood of selecting chromosomally normal embryos,” Dr. Desai says. “This is an intriguing possibility and we hope to exploit such information to help our patients!”
“The adoption of a single embryo transfer policy is imperative for the health of our patients and their babies,” she states. “However, this demands not only optimization of culture technology, but also embryo selection /deselection techniques.”
Development of noninvasive screening methods to assess embryo viability and implantation potential is the newest challenge in IVF and imperative as we continue to encourage elective single-embryo transfers. Cleveland Clinic is committed to this goal and is using its expertise and cutting-edge technology to continue to advance in this area.
Advertisement
References:
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment