Physicians and patients should discuss risks, benefits, expectations
By Turgut Bora Cengiz, MD, and Emre Gorgun, MD, FACS, FASCRS
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Aspects of modern life that may promote hemorrhoids include increased consumption of processed foods, a sedentary lifestyle and using cell phones while defecating, which translates to much more time spent on the toilet.
Hemorrhoids accounted for more than 3.5 million U.S. outpatient visits in 2010, and they were the third leading cause of hospital admissions related to gastrointestinal disease.1
Here, we review the process for diagnosing and grading hemorrhoids, as well as for selecting the appropriate medical or surgical treatment based on the most recent clinical evidence.
Hemorrhoids are the distal prolapse of the arteriovenous bundle, muscle fibers and surrounding connective tissue as an envelope below the dentate line in the anal canal. They usually present with painless rectal bleeding.2
The diagnosis of hemorrhoids relies on history and physical examination rather than on laboratory testing or imaging studies. Typically, the presenting symptom is painless rectal bleeding associated with bowel movements, usually appearing as bright red blood on the toilet paper or coating the stool. Severe itching and anal discomfort also are common, especially with chronic hemorrhoids.
A detailed patient history is important. It should include the extent, severity and duration of symptoms, frequency of bowel movements, associated symptoms (e.g., constipation, fecal incontinence), daily dietary habits and details of bowel movements (e.g., time spent during each bowel movement and concomitant cell phone use).3
Advertisement
Regarding bowel habits, some patients experience lifelong constipation or diarrhea. Therefore, what a patient considers a normal bowel habit may not be normal and should be investigated.4 Also, it is important to exclude external thrombosed hemorrhoids, anal fissure, anal abscess and Crohn’s disease.5
A digital rectal examination is the second step. During the examination, look for skin tags, sphincter tone, perianal hygiene and synchronous anal lesions.3 Of note, the Valsalva maneuver can be performed during the digital rectal examination.
Red flags for colorectal cancer on the digital rectal examination include a mass with or without presence of hemorrhoidal sacs and a bleeding source above the level of internal hemorrhoids.
Patients with recurrent abscesses, fistulas or skin tags (especially cauliflower-type skin tags) should be investigated for Crohn’s disease (Figure 1).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8885d4c3-a12d-49c6-b577-e43c1d1df9ac/20-DDI-011-Figure-1-880x560_jpg)
Figure 1. Patient with Crohn’s disease. Note the fistula orifices and skin tag.
Since rectal bleeding can be a sign of several diseases, including colorectal cancer, it is important to review any previous endoscopic results. Patients at high risk of colon cancer should undergo rigid proctoscopy, flexible sigmoidoscopy or colonoscopy.3,4 In our practice, we recommend endoscopic evaluation for patients older than age 40 with rectal bleeding, especially if they have a family history of colorectal cancer.
Hemorrhoids can be categorized as either external or internal.
External hemorrhoids are distinguished by their outer covering with perianal skin and anoderm and their location inferior to the dentate line. They are painful if the hemorrhoidal sac is occluded by a thrombotic clot.
Advertisement
Internal hemorrhoids are above the dentate line and covered with rectal columnar and transitional mucosa. They are further graded on a 4-point scale3:
In choosing the treatment for hemorrhoids, one should consider the disease grade and severity, its impact on the quality of life, the degree of pain it causes, the patient’s likelihood of adhering to treatment and the patient’s personal preference.
Regardless of severity, treatment almost always starts with a high-fiber diet and other lifestyle modifications that include bowel movement behaviors. This requires practitioners to spend significant time on patient education, regardless of the type or severity of the disease.
Treatments can be grouped in three categories: conservative, office-based and surgical. Practitioners should thoroughly discuss the options with the patient, emphasizing the pros and cons of each.
Conservative measures are aimed at softening the stool, relieving pain and correcting bad toileting habits. In most cases, the primary precipitating factor is lifestyle, and unless patients change it, they are more likely to have recurrent symptoms in the long term.
People take their phones into the bathroom, and this habit is blamed for increasing the time on the toilet and leading to increased pressure on the anal region and straining during defecation. Some research points to a direct correlation between the time spent on the toilet and hemorrhoidal disease, although the exact cause-and-effect relationship with cell phone use has not been determined. In general, spending excessive time on the commode, including reading, should be discouraged.
Advertisement
Johannsson et al6 reported that patients with hemorrhoids spent more time on the toilet and had to strain harder and more often than controls in the community and hospital.
Garg and Singh7 and Garg8 use the mnemonic “TONE” for appropriate defecation habits:
Fiber draws water into the lumen of the colon, increasing the water content of the stool. Recommended daily fiber intake is about 28 g for women and 38 g for men.9 This high level of intake is hard to achieve without supplements for someone who consumes a classic American diet with a lot of fast food.
Fiber supplements are strongly recommended in the American Society of Colon and Rectal Surgeons (ASCRS) practice guidelines3 based on a Cochrane review.10 In this meta-analysis, with fiber supplements the relative risk of persisting or nonimproving symptoms was 0.53 (95% confidence interval [CI] 0.38-0.73) and the relative risk of bleeding was 0.50 (95% CI 028-0.89). Psyllium husk is an inexpensive bulk-forming fiber supplement; the optimal daily dosage is not known.
We recommend at least 28 g of daily fiber intake for women and 38 g for men, for which psyllium husk can be used to complement the diet.
Laxatives such as docusate are used to change the stool consistency when there is an organic bowel problem rather than a dietary issue. They can be used as a complementary treatment to enhance the effect of the fiber treatment.
Advertisement
Topical anesthesia (e.g., 5% lidocaine) is commonly used to treat pain from low-grade lesions, but no reliable data have been published. As most cases of hemorrhoids tend to progress over time, one should not expect long-term improvement with topical anesthesia. Nevertheless, it can be used as an ancillary treatment in select cases when short-term improvement is the main goal, and we recommend it based on our own experience.
Hygiene. Bidet use or cleaning the perianal area with water is recommended.
Phlebotonics contain a variety of ingredients including natural plant extracts such as flavonoids and synthetic products. Even though the exact mechanism of action is not known, phlebotonics are thought to increase venous and lymphatic drainage, normalize capillary permeability and decrease inflammation in the hemorrhoidal cushions.4,11–13
In a Cochrane review of 24 randomized controlled trials, Perera et al14 found that phlebotonics improved the outcomes of:
Although phlebotonics give better results than placebo in the short-term management of hemorrhoids, there is a paucity of long-term data. Thus, the ASCRS clinical practice guidelines give the regular use of these agents only a weak recommendation.3
Flavonoids (diosmin, hesperidin, rutoside), in a meta-analysis vs. placebo in 1,514 patients, showed a beneficial response in terms of bleeding (relative risk [RR] 0.33), pruritus (RR 0.65) and recurrences (RR 0.53).15
Although Preparation H is commonly used as an over-the-counter medication, there are no good data on it and it is not considered a phlebotonic.
Office-based treatments — rubber band ligation, infrared photocoagulation, and sclerotherapy — are commonly used for grade I, II and III hemorrhoids that have not responded to conservative management. The primary goal of these treatments is to decrease blood flow into the hemorrhoidal sac.
Even though office-based treatments are highly effective and major complications are uncommon, recurrence rates can be high, requiring patients to undergo additional treatments. Moreover, septic complications can occur so patients should be closely observed for fever and urinary problems. Pain is a common symptom after office-based treatments, and bleeding may also occur.
The ASCRS guidelines strongly recommend office-based treatments for patients with grade I and II hemorrhoids, and for some with grade III hemorrhoids.3
Ligating the apex of the hemorrhoidal cushion stops the arterial flow and causes the hemorrhoidal tissue to undergo necrosis (Figure 2). The ligation is performed above the dentate line, where the sensory nerve fibers differ from those found below the line; therefore, the operation causes less pain than one would expect. One or more hemorrhoidal cushions can be ligated at the same time, although increased pain, bleeding and vasomotor reactions have been reported with multiple banding during a single procedure.16,17
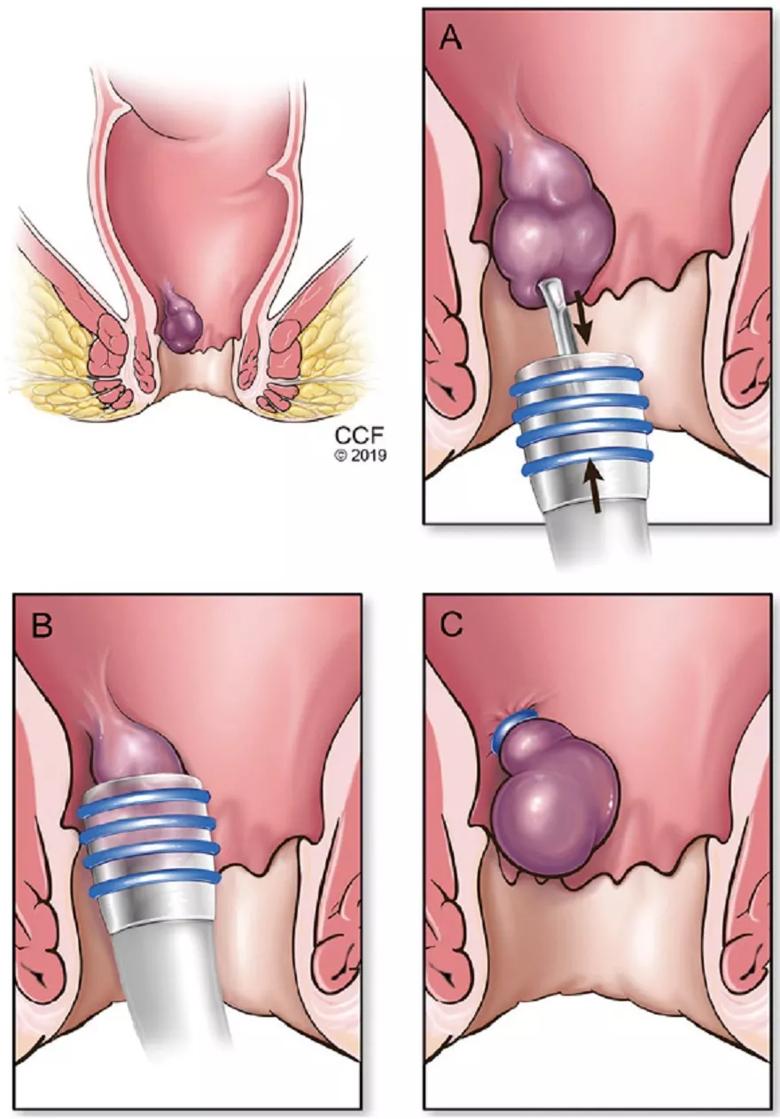
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d3a7ce5b-ce2d-4a76-aa70-2c85fa96144b/20-DDI-011-Figure-2-880x1500_jpg)
Figure 2. In rubber band ligation, an internal hemorrhoid is grasped with a forceps (A) and drawn into the cylinder of the ligator (B). A band is deployed around the base of the hemorrhoid (C), cutting off its blood supply and causing it to fall off within a few days.
Iyer et al18 reported that patients on warfarin therapy had as much as nine times higher risk of postprocedural bleeding, and patients on aspirin had a risk as much as three times higher. Therefore, whether patients on anticoagulant therapy should undergo this procedure is unclear.
A Cochrane database review19 found this technique effective for hemorrhoid grades I through III, although some patients with grade III hemorrhoids may benefit more from excisional hemorrhoidectomy, which is associated with a lower recurrence rate than rubber band ligation.
Brown et al20 performed a randomized controlled trial comparing hemorrhoidal artery ligation and rubber band ligation for symptomatic hemorrhoids in 372 patients with grade II and III hemorrhoids. Postprocedural pain scores on days one and seven were significantly lower with rubber band ligation, but recurrences were more common (49% vs 30%, p = .0005, respectively).
Overall, rubber band ligation is an excellent option for grade II hemorrhoids, as it is easy to perform, is associated with low pain scores and can be used to treat recurrences.
In this procedure, an infrared probe produces heat to induce coagulation, fibrosis and ultimately necrosis of the protruding tissue in the hemorrhoidal cushions.21 Even though its use was initially directed at grade I and II hemorrhoids, recent reports showed acceptable results for grades III and IV.22,23 A randomized controlled trial comparing infrared photocoagulation and rubber band ligation in 94 patients found that both procedures were well accepted and highly effective; however, patients had better pain scores with photocoagulation in the first 24 hours after the procedure (p < .05).24
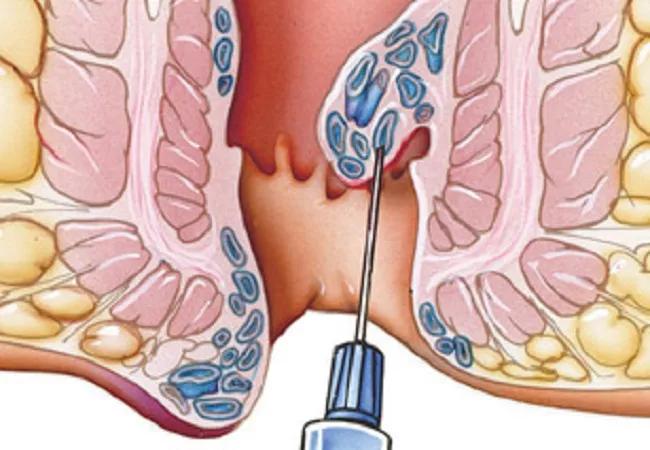
Sclerotherapy involves injection of a sclerotic agent into the submucosa of the hemorrhoidal sac (Figure 3), which causes an inflammatory reaction and eventually forms fibrotic tissue that stops the blood flow to the hemorrhoid. Many sclerotic agents are available, including 5% phenol in almond or vegetable oil, quinine, ethanolamine, and hypertonic saline.21
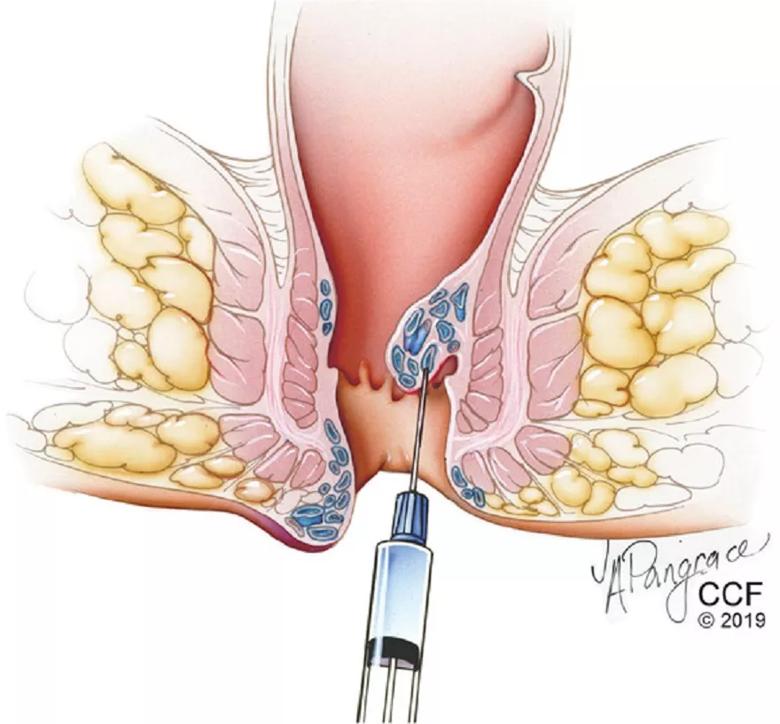
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a6ac896a-a3cc-4534-891f-31e673b64a0c/20-DDI-011-Figure-3-880x817_jpg)
Figure 3. Sclerotherapy involves injecting an irritating solution into the hemorrhoid, reducing its blood supply and causing it to shrink.
The injection can cause prostatic abscess and sepsis, although this is rare.25 Nevertheless, high fever and postprocedural pain should be carefully evaluated.
There have been few randomized trials of sclerotherapy, but success rates so far have been higher for grade I hemorrhoids than for grades II and III.26–28 It is the preferred method for patients who have bleeding abnormalities caused by medications or other diseases (e.g., cirrhosis).
Although nonsurgical treatments have substantially improved, surgery is the most effective and strongly recommended treatment for patients with high-grade internal hemorrhoids (grades III and IV), external and mixed hemorrhoids, and recurrent hemorrhoids.
The most popular surgical options are open or closed hemorrhoidectomy, stapled hemorrhoidopexy and Doppler-guided hemorrhoidal artery ligation. Each has different success rates and different complication profiles, which need to be discussed with the patient.
Overall, surgery is associated with more adverse effects than office-based treatments or medical management. Postoperative pain is the most common complaint, but anal stricture (rare) or incontinence may occur due to excessive tissue excision and damage to the sphincter muscles. These can be avoided by maintaining the normal anoderm between excisions, by not excising all hemorrhoid sacs at once if the patient has extensive lesions and by performing a careful dissection in the submucosal plane.
Patients with profuse bleeding or an underlying bleeding abnormality are best managed with surgical approaches performed in an operating room.
Excision of the hemorrhoidal sac, the most conventional surgical technique, is generally reserved for prolapsing disease. The recurrence rate after excisional hemorrhoidectomy is significantly lower than with any other approach.29
Excisional hemorrhoidectomy can be performed using either an open approach, in which the edges of the mucosal defect are not reapproximated, or a closed approach, in which they are. In a systematic review, Bhatti et al30 compared open vs. closed techniques and found that the closed technique resulted in less postoperative pain, better wound healing and less bleeding. Rates of recurrence, postoperative complications and surgical site infection and lengths of stay were comparable with either procedure.
Overall, excisional hemorrhoidectomy is associated with higher pain scores than any other surgical method.29 Recently, the use of electrodiathermy energy devices, also described as electrosurgical vessel-sealing devices, have further improved overall patient satisfaction.31
Multiple painful hemorrhoidal sacs require a careful surgical approach, as extensive resection may cause widespread fibrosis and stricture. As with anal stricture, fecal incontinence can be prevented by careful dissection. However, already existing incontinence is not a contraindication for the surgery.
Doppler-guided hemorrhoidal artery ligation involves using a Doppler probe to find and ligate individual hemorrhoidal arteries. Additionally, mucopexy (transanal rectoanal repair) is performed to relocate the prolapsing tissue. Avital et al32 reported that at one year after this procedure, recurrence rates were 5.3% for grade II hemorrhoids and 13% for grade III hemorrhoids. At five years, recurrence rates were 12% for grade II and 31% for grade III.
To date, this procedure appears to be suitable for grade I, II, and III hemorrhoids, especially for grade II, but more studies are needed to prove its efficacy and recurrence rates for more advanced lesions. Although this technique has a high morbidity rate (18%), primarily pain or tenesmus, it causes less postoperative pain than other surgical methods.33 Overall, it has the potential to become a favored treatment.
In this procedure, the prolapsing part of the internal hemorrhoidal cushion is moved upward by stapling the rectal mucosa just above the hemorrhoid (Figure 4). This is not an option for patients with thrombosed internal hemorrhoids or with external hemorrhoids.
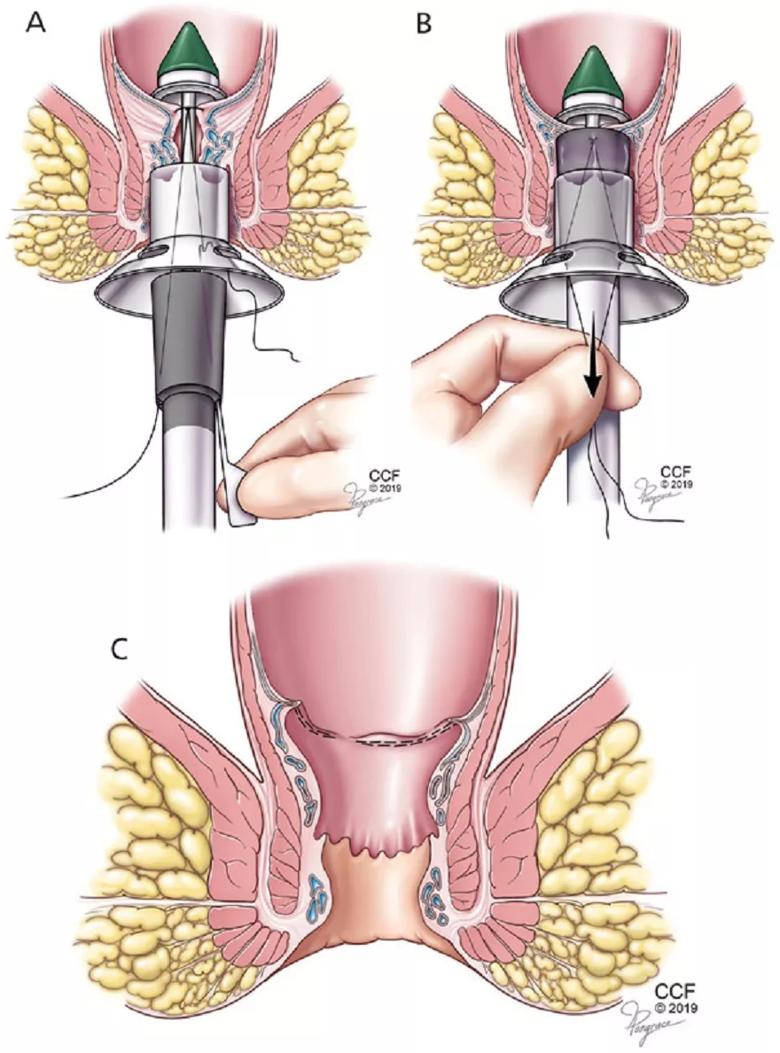
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6e44444a-f5de-4daa-81a6-054c84243486/20-DDI-011-Figure-4-880x1168_jpg)
Figure 4. In stapled hemorrhoidopexy, a special tool is inserted (A). Excess tissue is excised (B), and the remaining tissue is drawn up to its normal position and fastened in place, yielding the result pictured in panel C.
Although pain scores are lower with stapled hemorrhoidopexy than with excisional hemorrhoidectomy, this procedure is not superior in terms of recurrences.34,35 Also, practitioners should be careful about specific complications of stapled hemorrhoidopexy, such as rectovaginal fistula, anal stenosis or sphincter injuries. These specific complications should be clearly explained to patients, and necessary information should be given to patients upon discharge. The primary care physician should also be careful about fistulas and stenoses in this particular patient population.
There is no best treatment for hemorrhoids. Every patient is different, and the physician and patient need to understand each other’s expectations, weigh the risks and benefits and arrive at a mutual decision. A good patient-doctor relationship is essential.
A thorough history and physical examination will enable the practitioner to understand the patient’s problem (Figure 5).
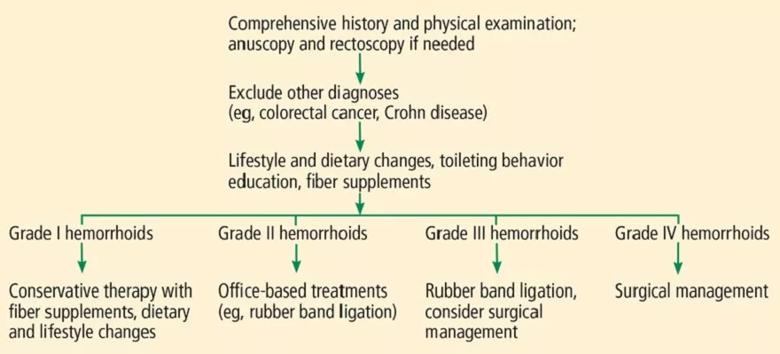
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ea169469-9458-4fcd-87b5-dce37253580e/20-DDI-011-Figure-5-880x399_jpg)
Figure 5. Algorithm for hemorrhoid management.
Given the variety of available treatments, head-to-head comparisons are difficult. Moreover, the efficacy and applicability of each technique changes with the grade of the lesion or lesions and the skill of the practitioner. Lacking comprehensive studies comparing conservative, office-based and surgical management, no decisive statements can be made based on current evidence.
Pregnant patients often develop hemorrhoids as intra-abdominal pressure increases, particularly during the third trimester.36 Also, acute episodes of pain and bleeding are common in pregnant women with preexisting hemorrhoids.
Conservative treatment is the main approach in pregnant patients because most hemorrhoids regress after childbirth. This includes increased dietary fiber, stool softeners and sitz baths, which are safe to use for external hemorrhoids. Any office-based or surgical intervention should be postponed until after childbirth, if possible. Kegel exercises and lying on the left side are also recommended to relieve symptoms. In cases of severe bleeding, anal packing appears to be useful.
Immunosuppressed patients and those on anticoagulant therapy are more prone to serious complications such as sepsis and profuse bleeding. Thus, conservative management should be used in these patients as well. Injection sclerotherapy may be beneficial, as it has been shown to decrease bleeding. Of note, patients on immunosuppressive agents should stop taking them and start taking an antibiotic, and patients on anticoagulant or antiplatelet medications should be instructed to stop them one week before any intervention.
Crohn’s disease. Some patients with Crohn’s disease may have hemorrhoids, though this is rare. Eglinton et al,37 in a series of 715 patients with Crohn’s disease, reported that 190 (26.6%) had symptomatic perianal disease. Of these, only 3 (1.6%) had hemorrhoids. Treatment is always conservative and directed at the Crohn’s disease rather than the hemorrhoids.
Patients with portal hypertension (e.g., due to cirrhosis) are prone to have anorectal varices that may resemble hemorrhoids. Anorectal varices can be treated with vascular ligation, whereas sclerotherapy is the preferred method for hemorrhoids in this group, in whom coagulopathy is common.
Hemorrhoidal disease is common in the United States, and with our diet and lifestyle, the incidence is likely to increase. (A national survey found that overall dietary quality improved modestly in children and adolescents in the United States from 1999 to 2012 but remained far below optimal.38) Practitioners need to carefully assess hemorrhoidal symptoms and complete any necessary screening tests before establishing a diagnosis. This helps to avoid missing any underlying disease.
Fiber supplements along with dietary and lifestyle changes constitute the baseline of the management, regardless of the disease grade. Office-based interventions are beneficial for grade I and II hemorrhoids and for some grade III hemorrhoids. Repeated interventions can increase the success rate. In patients with high-grade, symptomatic hemorrhoids, surgical hemorrhoidectomy is the most effective modality with the lowest recurrence rates, although it causes more pain than conservative methods.
Dr. Cengiz is a resident in Cleveland Clinic Digestive Disease & Surgery Institute’s Department of General Surgery. Dr. Gorgun is Director for Lower GI of the Digestive Disease & Surgery Institute’s Endoluminal Surgery Center.
Note: This article originally was published in the Cleveland Clinic Journal of Medicine (2019 September;86(9):612-620).
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years