Patients with overweight/obesity are as likely to experience disordered eating as their normal-weight peers
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Jeannette is a 22-year-old woman who presents with a chief complaint of fatigue. A history reveals that she has lost weight in the past 6 months — she used to weigh 220 lb but now weighs 180; her height is 5’4”. She lost weight by reducing her portion sizes, eliminating junk food and anything else “unhealthy,” attending a spinning class four days per week, and walking at least 10,000 steps every day, as recommended at her well visit a year ago when her body mass index (BMI) was 37.8 kg/m2. Her BMI is now 30.9 kg/m2. On examination, her heart rate is 50 beats per minute, and she has mild orthostatic changes in pulse but not in blood pressure. What do you think is going on?
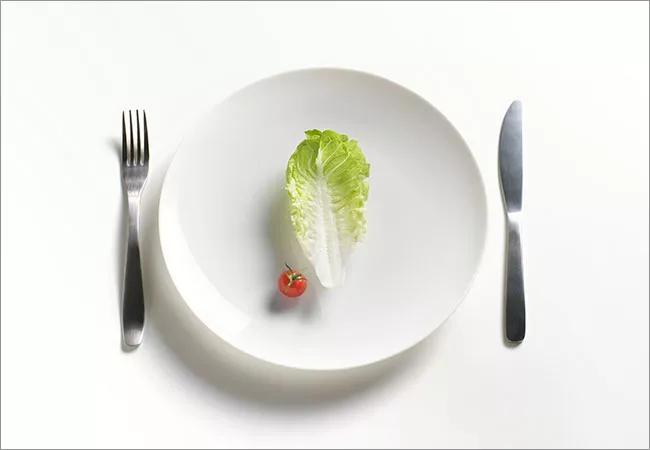
Some patients with restrictive eating disorders are hiding in plain sight. Although a patient who starts at 120 lb and loses 40 will look anorectic, someone who starts at 220 lb and comes in weighing 180 may not, despite losing the same amount of weight through the same disordered eating behaviors and putting herself or himself at the same risk of physical harm through starvation.
Patients who have overweight/obesity are in a tough position. We want them to lose weight, but we want them to do so safely. Restrictive eating disorders tend to be under-recognized in this group, even though research suggests that these patients may have a greater likelihood of disordered eating habits than those with no history of overweight/obesity. It is therefore important for primary care physicians to consider eating disorders in young patients at a variety of weights.
Advertisement
In adolescents and young adults with restrictive eating disorders, the prevalence of a history of overweight/obesity ranges from 19.3% to 36.7%.3–5 These numbers mirror the national prevalence of overweight/obesity, suggesting that patients with higher weight status are as likely to experience disordered eating as their normal-weight peers.4
Indeed, overweight adolescents report greater concern about their weight and more body dissatisfaction than their normal-weight peers.6 These concerns could lead them to engage in disordered eating behaviors, including bingeing, purging, and diet pill use.6–9 There is now a greater recognition of eating disorder diagnoses in young adults who may not meet low-weight criteria but otherwise have classic symptoms.
Although they present with a higher BMI compared with patients with anorexia nervosa or bulimia nervosa who started out in the normal-weight category, those who started out with overweight/obesity lose more weight (have greater “weight suppression”), whether the change is measured in kilograms, BMI, or percent body weight.3,4 The higher weight at presentation results in a more common diagnosis of atypical anorexia nervosa in these patients.3
The amount of weight suppression is a valuable indication of disease severity as well as a prognostic tool.3,4 A greater percent weight loss has been associated with worse psychological and physical symptoms in patients with anorexia nervosa.10,11 A position paper from the Society for Adolescent Health and Medicine has advocated for greater recognition of the clinical utility of percent weight loss and emphasizes the dual roles of weight status as well as rate and relative amount of weight loss.12
Advertisement
When the degree of weight suppression based on percent body weight loss is considered, then there is no difference in the likelihood of inpatient treatment, suggesting that weight suppression is a more appropriate metric of starvation state than absolute weight status.3
Previously overweight adolescents are less likely to receive inpatient treatment despite similar symptoms compared with their previously normal weight peers.3 This discrepancy has been attributed to the higher weight at presentation.3 This relationship was found to be mediated by weight suppression, supporting the trend toward assessing degree of weight loss rather than focusing primarily on presentation weight when evaluating for eating disorder symptoms.3
Comparisons of eating disorder symptom burden based on the Eating Disorder Examination-Questionnaire reveal that previously overweight patients have similar symptoms such as degree of restraint around food and concern about shape or weight.4 However, children with overweight/obesity are more at risk than their normal-weight peers of engaging in disordered eating behaviors and exhibiting unhealthy weight loss strategies.13
Finally, the duration of illness before presentation may be more variable. Two studies3,4 found that the duration of illness is significantly longer in patients with higher premorbid BMIs, whereas another reported that the duration of illness was comparable to that among healthy-weight peers who developed restrictive eating disorders.14 These discrepancies may be explained by differences in definitions or small sample sizes.
Advertisement
The malnutrition resulting from restrictive eating disorders affects every system in the body and can occur even in the face of obese or overweight status, as seen in the case of Jeannette. Consequences can be lifelong and include the following:
Advertisement
Although many people with overweight/obesity people have eating disorders, most research is limited to underweight patients only.23,24,32 Thus, there are few data to guide management of weight loss-related sequelae in previously overweight patients presenting with eating disorders.
In general, body fat mass, amount of relative weight loss, and appropriate hormonal levels and interactions contribute to normal menstrual function.33,34 Disruption of the hypothalamic-pituitary-ovarian axis by weight loss may be mediated by changes in gonadotropin-releasing hormone (GnRH) release. Typical GnRH function is pulsatile and relies on leptin and insulin-like growth factor 1 (IGF-1) signaling.35–37 Fat mass contributes to normal production of both leptin and IGF-1, and therefore loss of fat mass can disrupt the hormonal signaling underlying normal menstruation.22,38,39
Previously overweight patients follow a different course than their previously healthy weight peers in menses recovery. In one study, amenorrheic patients with a history of overweight/ obesity resumed menses at a higher weight but with similar amounts of absolute gain in weight.5 Additionally, the likelihood of menses resumption decreases with greater weight suppression and increases with greater weight gain during treatment in both groups.5
This finding suggests that weight goals associated with resumption of menses may need to be higher for patients with a history of overweight. Weight restoration may therefore have different effects on adolescents who had different baseline hormonal production, given different fat mass before the onset of illness. The difference in patterns of menses resumption highlights the need to identify physiologic alterations that may differ between previously overweight and previously normal-weight teens at the onset of eating disorders.
That only one study has compared outcomes between adolescents and young adults with eating disorders by premorbid weight status shows the understudied nature of this comparably high-risk population. While there is greater recognition of the differences in the population, there remains a paucity of studies on treatment goals and recovery course, making it difficult to use evidence-based medicine to assess response to treatment.
Until definitive guidelines are published, the primary care physician can use the following general treatment advice:
Jeannette returns after 1 month, having seen the dietitian and increased her intake to 1,800 kcal per day from her previous 400 to 600 kcal per day. Her weight is now 185 lb. Her heart rate has increased to the 60s, but she has ongoing amenorrhea. Her luteinizing hormone level is 2.0 mU/mL and her follicle-stimulating hormone level is 2.6 mU/mL. These values are on the low-normal side, consistent with functional hypothalamic amenorrhea, in which there is suppression of gonadotropins that is centrally mediated through the release of GnRH from the hypothalamus. Her thyroid-stimulating hormone level is normal, and her white blood cell count has normalized (she was previously mildly leukopenic).
Note: This is an abridged version of an article originally published in the Cleveland Clinic Journal of Medicine. To view the entire article, along with a complete list of references, please visit https://www.ccjm.org/content/87/3/165.
Advertisement

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve