Implementing standardized tools across an 18-hospital system

In 2018, Cleveland Clinic began an enterprise-wide upgrade of its Epic software, giving clinicians access to the most up-to-date and sophisticated technology available and thus ensuring Cleveland Clinic’s promise of delivering a world-class patient experience. An electronic health record (EHR) upgrade of this nature is no small task for a global health system like Cleveland Clinic, which has > 210 outpatient locations, 18 hospitals and approximately 66,000 caregivers worldwide (as of January 1, 2019).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To learn more about the upgrade and how it impacts patients and providers, as well as the change management process itself, Consult QD sat down with Amy Merlino, MD, Enterprise Chief Medical Information Officer and a practicing maternal-fetal medicine specialist.
Dr. Merlino: The basic concepts of the EHR transformation program are to get our clinical technology (Epic) up to the current state, and standardized across our organization. EHR tools have improved significantly over the years, so a certain amount of updating is required just to keep up. Additionally, some of our homegrown systems have become obsolete, or don’t integrate well with the rest of the record.
For example, our anesthesia department developed an electronic recordkeeping system for medications administered in the operating room long before Epic and others were in the market. At the time, it was very innovative. Once Cleveland Clinic adopted Epic, these anesthesia records were added to patient charts as PDF attachments. Although the records were saved, they weren’t really integrated with the patient record.
The key objective of EHR transformation is to ensure that all Cleveland Clinic patients are getting the same, high-quality care, regardless of where they receive care.
That isn’t to say that the EHR will look the same to all caregivers in all specialties. Specialty transformation is important too, as each caregiver has a different part of the picture that’s important to them. We will be looking at both the ambulatory and inpatient tools that our caregivers use, and customizing the initial screens so that the information they need — the data that means the most for the care they provide for their patients — is presented first. So, what a cardiologist sees on those initial screens should be different from what an endocrinologist sees.
Advertisement
In order to be successful, we need input from our clinical providers. This project is really a partnership with the organization. We needed clinicians to help us understand what information they need, and how it is used to provide patient care. It has been a fairly lengthy process of evaluation from multiple inputs in order to identify the core scope of our work. Our goal is to present the information in a meaningful and intuitive way from the start, so that caregivers can care for patients rather than hunting through the EHR for information.
Dr. Merlino: At the outset, we earned the support of Cleveland Clinic’s executive leadership, and the Institute leaders helped to identify groups of caregivers who could represent their departments. We work with these superusers, if you will, shadowing them to learn how they use the EHR, in order to develop an understanding of their painpoints. We look for opportunities for improvement, and then compare those against the list of standard Epic tools that we have not yet deployed.
Once we have about 90% of the picture, we hold open forums where anyone who might be the recipient of these new tools can try them out, and let us know if we missed the mark.
Additionally, we’re finding through this process that there are operational differences between our sites. There’s always the opportunity for sharing best practices, and continued training to ensure we are making the best use of the tools that are available to us.
Dr. Merlino: That’s our goal, and one that we think will help us deliver world-class care everywhere. Using standard tools also helps our IT teams to be more efficient. If we’re not the same everywhere, we have to manage how changes will be deployed at each hospital. That doesn’t allow us to meet the needs of a growing organization. This transformation gives us a solid foundation of standardized best practices to we can build upon and scale as we grow.
Advertisement
Dr. Merlino: We are deploying by region, starting with hospitals and core facilities located in our west market, then moving to the east and south markets, Florida and London. This structure allows us to have dedicated support staff onsite at each go-live event to help with change management and training. In certain specialties that will be receiving entirely new modules, such as our anesthesia department, we will train clinical champions first, so that our caregivers can support each other. We will also provide elbow support, and classroom and online training.
Dr. Merlino: Most of the tools we’re deploying are to users who have been using Epic for a while, and the majority of the changes are enhancements that do not require a significant amount of training. Those users who want to engage by taking the training and getting the elbow-support they need during deployment, will find many benefits. Those who do not engage will still be able to work as before. When we encounter clinicians who are resisting these changes, we often find those conversations lead us to better changes because their concerns are valid. If not, those conversations are an opportunity to try to help them understand the value we’re trying to bring them.
Dr. Merlino: Success will mean that we have optimized our EHR across the organization in a standardized way, the tool is meeting the needs of our caregivers, we stay on budget, and we are able to use the EHR to extend the Cleveland Clinic brand and care as we grow in other locations.
Advertisement
We have had some early wins on the specialty transformation front. We started with the Neurological Institute, for which we have rolled out several specialty-specific tools. Physicians in this group have found value in the tools we’ve rolled out. We’ll also be looking at metrics from ambulatory providers, including basic usage of items to ensure that the tools we are rolling out are the right ones. Additionally, we will look at the data we have on how much time our caregivers are spending within the medical record. We are always cautious when we look at this metric — we want providers to spend time in the EHR as it’s an important aspect of the care they provide. But, if we can get caregivers to interact with the computer and the record together in an intuitive way, we hope to decrease the amount of time folks might have to spend circling back on the documentation after hours.
Advertisement
Advertisement

Advanced software streamlines charting, supports deeper patient connections

How holding simulations in clinical settings can improve workflow and identify latent operational threats

Interactive Zen Quest experience helps promote relaxing behaviors

Cleveland Clinic and IBM leaders share insights, concerns, optimism about impacts
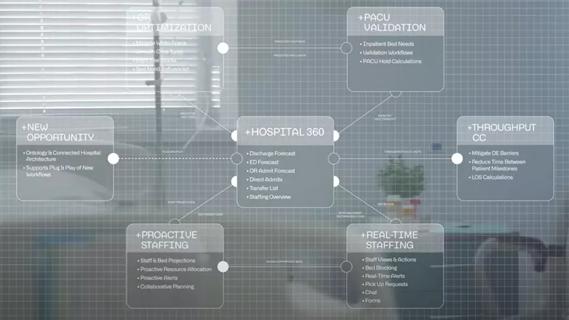
Cleveland Clinic partners with Palantir to create logistical command center

A Q&A with organizational development researcher Gina Thoebes

Cleveland Clinic transformation leader led development of benchmarking tool with NAHQ

Raed Dweik, MD, on change management and the importance of communication