Cultural changes, visual schedule boards and huddles drive ongoing improvement

By Andre Machado, MD, PhD; Steven Shook, MD, MBA; and Lisa Yerian, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Promoting a culture of improvement across a healthcare organization means empowering all caregivers to make improvements every day. This culture was recently brought to bear in Cleveland Clinic’s Neurological Institute to increase capacity in our neurosurgery operating rooms (ORs) to better meet patient needs.
Cleveland Clinic’s reputation for treating patients with the most complex cases of brain and spine disease resulted in a dilemma in recent years: We increasingly struggled to meet growing patient demand for certain neurosurgical procedures with optimal timeliness, resulting in frustration for patients and stress for caregivers.
In response, teams in our Neurological Institute identified a need to increase our neurosurgery OR capacity by 20 percent in order to perform more surgeries for patients with complex brain and spine conditions. These operations can last a few hours to a full day, with patients discharged immediately or remaining in the hospital for up to 10 days.
The goals of our initiative were to:
We aimed to apply four core elements of the “Cleveland Clinic Improvement Model” originally developed in 2014 to aid the organization in advancing a culture of improvement:
Advertisement
Specific changes began with collecting data on — and then visualizing — the entire OR scheduling process. Central to this was creating visual surgery schedule boards (see photo below) showing which cases are scheduled in which ORs for the upcoming nine weeks. These boards reveal times of open capacity and allow neurosurgery teams to quickly identify problems and proactively manage cases to fill the OR schedule without overwhelming caregivers.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dd594d09-e747-4285-a855-e90d23a38dd3/18-NEU-5807-Neuro-OR-Schedule-1_jpg)
The scheduling team now uses the boards daily to understand our OR capacity and demand. The boards serve as the meeting spot for twice-weekly team huddles to identify and solve problems such as gaps in the schedule or overbooked days. Nursing and physician leaders join with care coordinators to assist the scheduling team by removing scheduling obstacles and providing support to overcome any recurring problems.
Introduction of the schedule boards and regular huddles was accompanied by standardization of key OR scheduling procedures to complete the revised approach to scheduling.
These OR scheduling changes were introduced in February 2018. An analysis of impact through September 2018 showed a consistent improvement in neurosurgery OR utilization within the first seven months under the changes, as detailed in the graph below. Notable specific findings included:
Advertisement
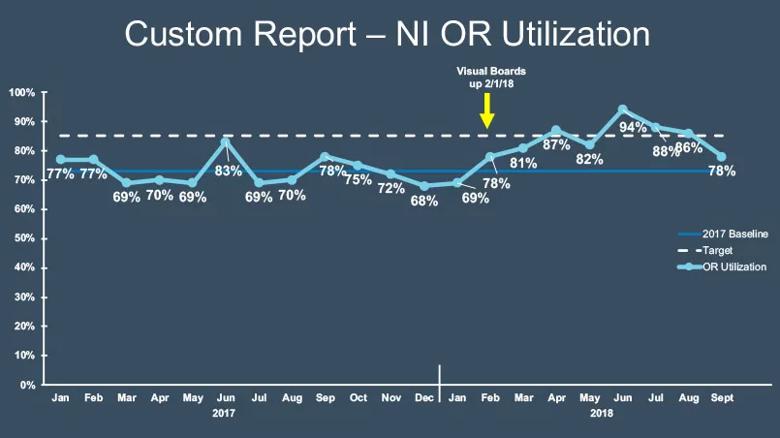
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6e43efb5-bd0b-4fdd-9992-b754f2a3f7ac/18-NEU-5807-Neuro-OR-Schedule-2_jpg)
Other benefits ensued as well. The analysis through September 2018 showed the following:
The results observed in recent months suggest that the revisions made to our OR scheduling process have allowed us to do the following:
Many details of the changes outlined above were suggested by individual caregivers of various levels of training and responsibility both before and during the institution of regular huddles. Indeed, one of the key objectives of huddles is to foster such suggestions on an ongoing basis to make continuous improvement a consistent reality.
While further improvements remain to be made, the above results signal that we are on the right path toward optimizing our OR scheduling practices to better serve our patients and caregivers. We will continue to engage and empower our caregivers every day to make ongoing improvement the norm for the betterment of patients and providers alike.
Dr. Machado is a neurosurgeon and Chair of the Neurological Institute. Dr. Shook is a neurologist and Vice Chair of Operations and Quality Improvement Officer for the Neurological Institute. Dr. Yerian is a pathologist and Medical Director of Continuous Improvement at Cleveland Clinic.
Advertisement
Advertisement

Advanced software streamlines charting, supports deeper patient connections

How holding simulations in clinical settings can improve workflow and identify latent operational threats

Interactive Zen Quest experience helps promote relaxing behaviors

Cleveland Clinic and IBM leaders share insights, concerns, optimism about impacts
Cleveland Clinic partners with Palantir to create logistical command center

A Q&A with organizational development researcher Gina Thoebes

Cleveland Clinic transformation leader led development of benchmarking tool with NAHQ

Raed Dweik, MD, on change management and the importance of communication