Researchers hope it may one day help patients avoid explantation surgery
The main cause of morbidity and mortality in periprosthetic joint infection (PJI) may be the treatment: revision surgery. A team at Cleveland Clinic and Case Western Reserve University is searching for ways to make explantation surgery unnecessary by treating PJI while preserving the prosthesis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“PJI is difficult to treat because of a biofilm that shields the bacteria from antibiotics and the patient’s immune response,” says Carlos Higuera-Rueda, MD, Director of the Levitetz Department of Orthopaedic Surgery at Cleveland Clinic Weston Hospital. “If we can find a way to break through the biofilm, antibiotic treatments will be more effective.”
For a little over eight years, Dr. Higuera-Rueda and colleagues in Cleveland Clinic Adult Reconstruction Research and Case Western Reserve University’s Department of Chemistry have been developing an amino acid substance to do just that. What started as a test on titanium disks and chicken breast has progressed to studies on in vivo models. The team’s most recent work — a study that showed a significant decrease in implant biofilm and infection in a model of knee PJI — was honored with The Knee Society’s Mark B. Coventry, MD, Award at the American Academy of Orthopaedic Surgeons (AAOS) 2024 meeting.
“Earlier work showed that our anti-biofilm treatment, PhotothermAA gel, completely eradicated two-week-old mature biofilm in vitro,” says Dr. Higuera-Rueda. “Our latest work showed its efficacy in vivo, when combined with debridement, antibiotics and implant retention.”
Conventional treatment of PJI is marginal at best, says Dr. Higuera-Rueda. The biggest reason is the formation of biofilm, a biomatrix built by bacteria that is difficult to disrupt mechanically or chemically, including with antibiotics. Today, thoroughly removing the biomatrix requires removing the entire implant.
Advertisement
In the U.S., after removing the implant, surgeons typically insert a spacer, most often made of cement with a high concentration of antibiotics. These rigid spacers can cause pain for the patient and restrict their range of motion. Patients usually have the spacer for two to three months, during which time they receive antibiotics. After that, they have another surgery to place a new prosthetic joint, followed by months of recovery.
It can take six months for a patient to go through the whole process, says Dr. Higuera-Rueda. And still, successful outcomes are as low as 66%, according to some research. Many revision surgeries are not successful, sometimes leading to more surgery, limb loss or even death.
“The five-year mortality after septic revision is 26% — higher than the mortality rate of most common cancers,” says Dr. Higuera-Rueda. “Since hip and knee replacements in the U.S. are growing exponentially, finding a viable alternative to the way we currently treat PJI would have a sizeable impact.”
One anti-biofilm solution being developed by Dr. Higuera-Rueda and colleagues is PhotothermAA gel, which combines D-amino acids (tryptophan, tyrosine and phenylalanine) and gold nanoparticles. The solution changes consistency according to temperature: liquid when cold, gel when warm.
This form-changing feature is important. When applied to the open joint, the gel solution congeals around the prosthesis rather than flowing into soft tissue where it could cause damage when activated.
“We have tested different catalyzers,” says Dr. Higuera-Rueda. “We tried using an electromagnetic field, but it increased the temperature too abruptly, causing some burning in soft tissue. We found that a laser provided a more gradual and safer temperature increase.”
Advertisement
As the temperature of the hydrogel rises, D-amino acids are released, disrupting the covalent bonds within the bacterial biofilm.
“Our solution, when heated, creates holes in the biofilm matrix so it’s easier for antibiotics to get in,” explains Dr. Higuera-Rueda.
There are multiple anti-biofilm treatments in development, he notes, but no others in gel form.
The research team published on the effectiveness of PhotothermAA gel in vitro in 2020 and 2023. The study presented at AAOS 2024, and recently published in The Journal of Arthroplasty, was the first to show effectiveness in an animal model of knee replacement (titanium tibial implant) that became infected.
The team studied three groups of models, one treated with surgical debridement and antibiotics; one treated with surgical debridement, antibiotics and PhotothermAA gel; and one control group. They reported that when compared to treatment without the gel, models treated with the gel had:
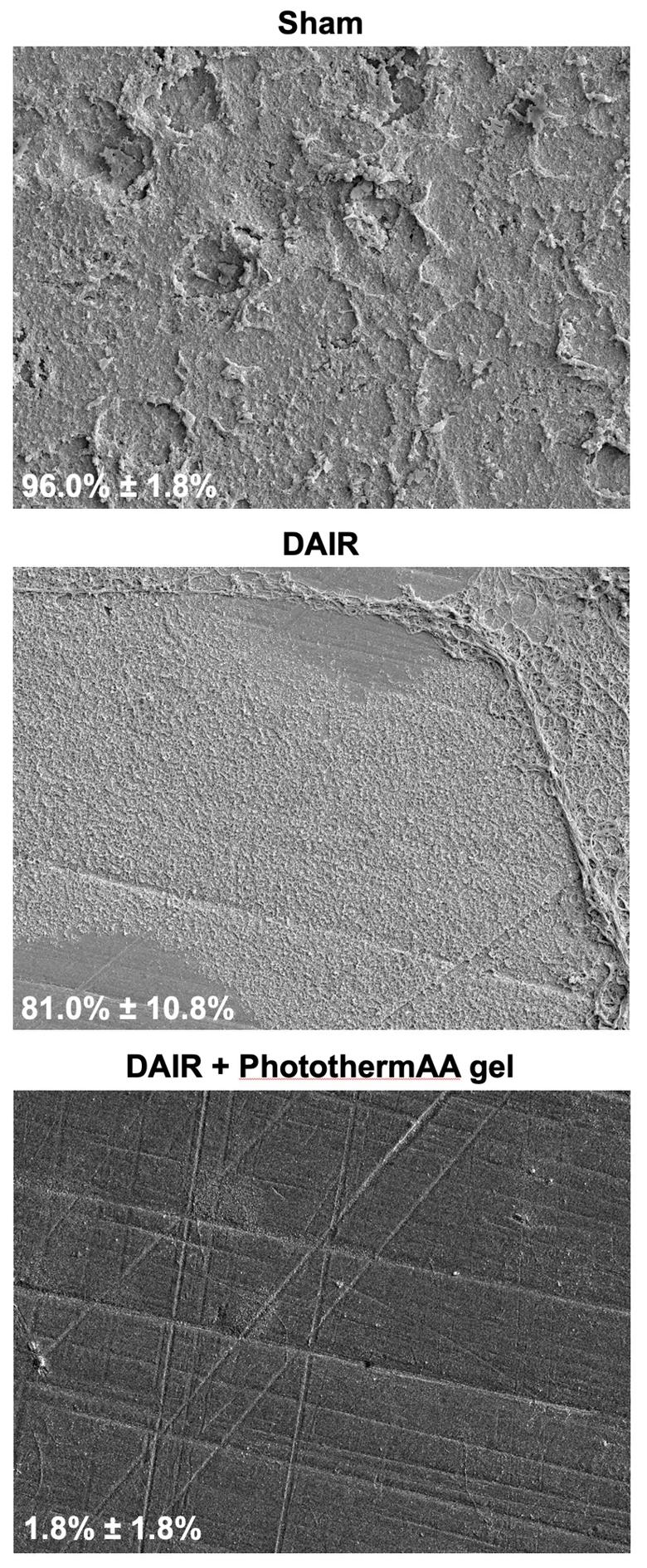
Image content: This image is available to view online.
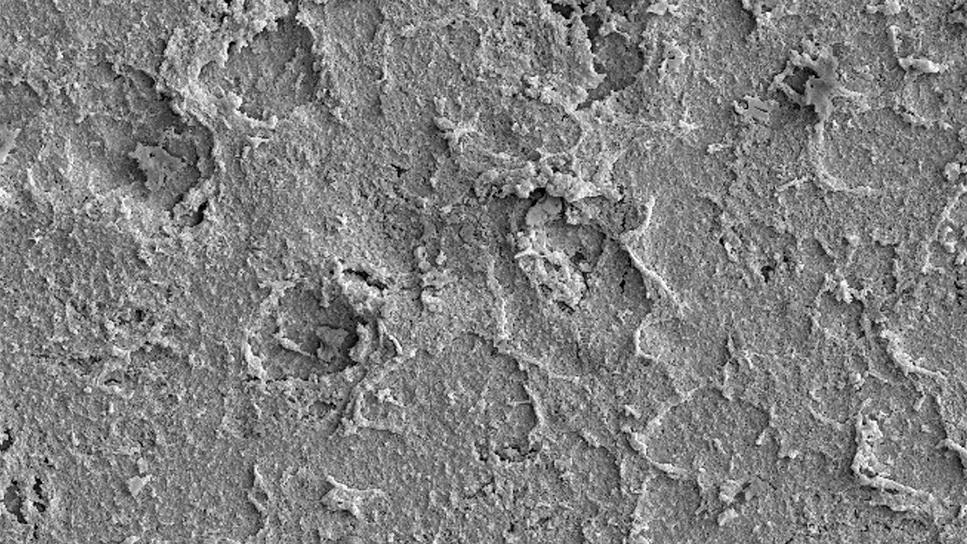
View image online (https://assets.clevelandclinic.org/transform/2f5adab9-e393-4194-a0e6-f57b1f348149/biofilm-on-scanning-microscopy-feature-inset)
Scanning electron microscopy images of bacterial biofilm coverage at 1500x magnification two weeks after treatment. Average coverage is mean ± SEM (standard error of the mean) of 20 predefined locations per implant surface.
The gel-treatment procedure involved:
1. Surgery to open the infected joint
2. Debridement to remove necrotic tissue and purulence
3. Application of the gel, including an incubation period followed by 10 minutes of laser exposure
4. Saline wash to remove the gel
5. Closure of the surgical incision
Advertisement
6. Administration of systemic antibiotics
“We have collected good efficacy data, showing that our gel can facilitate treatment of PJI in a much less invasive way, allowing the prosthesis to be retained,” says Dr. Higuera-Rueda, the study’s first author.
The team now is working on gathering more safety data. They aim to expedite the incubation time, hoping to reduce it from two hours to 30 minutes or less. They also are exploring if washing out the gel with an antimicrobial solution would complement the process.
“In my view, PJI is like cancer,” says Dr. Higuera-Rueda. “If you leave any malignant cells behind, it can come back. For that reason, we have shown the robust effect of our solution with electron microscopy, scanning implant surfaces rather than just relying on colony forming unit measurements. Our PhotothermAA gel shows great promise for the future of PJI treatment.”
Advertisement
Advertisement

Collaboration must cross borders and disciplines

Clinical complexity demands personalized care strategies

Higher than 5-year rates for prostate cancer and melanoma and about the same as breast cancer

Sinus tracts can occur years later and not near the incision site

Symptoms complement one another

How to diagnose and treat crystalline arthropathy after knee replacement

How it’s similar but different from the direct anterior approach

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols