Orthopaedic surgeons discuss their recently funded National Institutes of Health R01 grant

Written by Eric T. Ricchetti, MD; Kathleen A. Derwin, PhD; Joseph P. Iannotti, MD, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The number of shoulder arthroplasty procedures performed in the United States continues to rise, with current estimates ranging from 55,000 to 80,000 per year and increases of 300% or more expected in the coming years. While total shoulder arthroplasty (TSA) is the preferred surgical treatment for advanced glenohumeral arthritis, a subset of patients do not experience clinical improvement or sustain a complication. Glenoid component loosening is reported as the most common long-term complication of anatomic TSA and a common reason for revision surgery.
In addition, the factors associated with poor short- and long-term clinical outcomes after anatomic TSA are still not well understood, in part due to the lack of large prospective cohort studies allowing for multivariable analysis. Furthermore, while an association between glenoid component loosening on plain radiographs and worse clinical outcomes, including the need for revision surgery, has been shown at longer follow-up, the significance of early radiographic changes on longer-term clinical outcome has not been established, nor have the factors associated with glenoid component loosening been well-defined. The ability to reliably and accurately measure subtle radiographic factors longitudinally following anatomic TSA may allow for a deeper understanding of the relationship between short- and longer-term clinical outcomes.
The objective of our recently funded National Institutes of Health R01 grant is to identify the factors associated with short- and longer-term clinical and radiographic outcomes following anatomic TSA by utilizing two unique and ongoing prospective TSA cohorts: a larger cohort (over 1,200 projected cases) collecting baseline demographic, disease-related and surgical factors, together with one-year clinical outcomes, and a smaller cohort (N = 152) collecting CT imaging-based measures, as well as minimum five-year clinical outcomes. The central hypothesis is that short-term (one-year) outcomes will associate with certain demographic, disease-related and surgical factors, while longer-term (minimum five years) outcomes will associate with the factors influencing short-term outcomes, as well as radiographic changes that may be clinically silent in the short-term, in particular glenoid component shift and central anchor peg osteolysis at a minimum two-year follow-up.
Advertisement
An innovation in this grant is the ability to investigate a large prospective cohort of patients undergoing primary anatomic TSA for glenohumeral osteoarthritis (over 1,200 projected cases) with multivariable analysis through the Outcomes Management and Evaluation (OME) system at Cleveland Clinic. OME provides a valid, scalable, cost-effective and prospective data collection tool for assessment of clinical outcomes with a high rate of post-operative follow-up.1 OME will be used to assess the extent to which 20 baseline demographic, disease-related and surgical factors are associated with patient-reported outcomes at one-year post-operatively. We hypothesize that certain factors will independently associate with one-year patient-reported outcomes (Penn Shoulder Score [PSS], Single Assessment Numeric Evaluation score [SANE]), after controlling for the other factors, and develop predictive models for these one-year clinical outcomes.
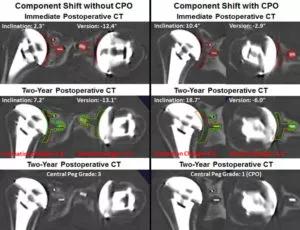
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/626fb8ae-84c5-4ac0-96f8-0c6b335330e3/20-ORI-1958832-CQD-Outcomes-Following-Total-Shoulder-Arthroplasty-Inset-300x230_jpg)
Another innovation is the use of previously validated novel methods of three-dimensional (3D) imaging analysis using widely accessible CT scanning together with metal artifact reduction (MAR) techniques that allow for reliable and accurate determination of implant position of a polyethylene glenoid component following TSA, with the ability to detect subtle changes in both over time.2-6 These methods allow the assessment of pre-operative bony pathology and post-operative implant position, as well as detailed information of other structures, including the rotator cuff and bone-implant interface, which may contribute to implant longevity and clinical outcomes. Our unique cohort of 152 anatomic TSA patients has been followed with sequential 3D CT imaging analysis to two years post-operatively. This cohort will allow investigation of whether early evidence of glenoid component shift, which cannot be detected by standard x-rays, will predict later, more obvious component loosening and/or premature clinical failure seen at a minimum of five years after surgery. We will conduct analyses of the incremental contribution of CT imaging-based radiologic factors to the prediction of longer-term clinical outcomes at a minimum of five years after primary anatomic TSA, including glenoid component shift and central peg osteolysis, beyond that provided by the perioperative risk factors identified in the larger OME cohort.
Advertisement
We expect to address gaps in prior literature by utilizing these two unique prospective anatomic TSA cohorts to simultaneously investigate the factors that associate with short- and longer-term clinical outcomes following anatomic TSA. Identifying risk factors that are important to clinical outcomes would allow for the design of future prospective clinical trial(s) to investigate modification of these factors either directly or indirectly through preoperative intervention or modification of surgical treatments and/or patient selection based on these factors, with the aim to improve outcomes and survivorship following anatomic TSA.
About the Authors
Dr. Ricchetti is a staff orthopaedic surgeon and Center Director for Shoulder Surgery in the Department of Orthopaedic Surgery. Dr. Derwin is staff at the Lerner Research Institute and Director of the Cleveland Clinic Musculoskeletal Research Center. Dr. Iannotti is Interim CEO & President, and Chief of Staff of Cleveland Clinic Florida.
Advertisement
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment