The tool can provide better clarity on evaluation of indeterminate thyroid nodules, reduce the number of unnecessary surgeries and help providers tailor patient care
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8e4034f4-2a3d-472b-8606-686d54777851/22-EMI-3244443-CQD-molecular-profiling-image_jpg)
Dr. Joyce Shin demostrating a thyroid ultrasound and exam with patient.
Thyroid nodules are particularly common, and by the age of 60, more than half the population will have been affected by them. While most thyroid nodules are not serious, a small percentage are cancerous. A fine needle aspiration (FNA) biopsy is the most accurate and cost-effective procedure for evaluating thyroid nodules; however, about one-third of nodules have indeterminate cytology, which is associated with a small but significant malignancy risk. When thyroid nodules are malignant, thyroidectomy is the standard treatment, but there are several associated risks (hypoparathyroidism, vocal change, infection and bleeding). Over the past few years, molecular profiling has emerged as a strong option for thyroidologists to diagnose indeterminate nodules better and reduce unnecessary surgeries.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
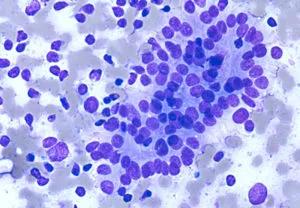
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ea989eda-4e21-4d2a-87e3-5b381fb9b18e/22-EMI-3244443-CQD_EN-Molecular-Profiling-scan-300x208_jpg)
Atypia of Undetermined significance. Follicular cells with crowding and pseudo-stratification are shown.
The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) is used to help classify and standardize nodules based on FNA specimens. The system includes six diagnostic categories: (I) nondiagnostic or unsatisfactory; (II) benign; (III) atypia of undetermined significance (AUS) or follicular lesion of undetermined significance (FLUS); (IV) follicular neoplasm or suspicious for a follicular neoplasm; (V) suspicious for malignancy; and (VI) malignant.
If a nodule falls into Bethesda III or IV categories, the Afirma Genomic Sequencing Classifier (GSC) can be used to gather more information about the nodule. GSC analyzes the mRNA expression of 167 gene patterns along with RET, BRAFV600E, and RET/PTC1/3. The Afirma Xpression Atlas (XA) expands upon the GSC insights and includes certain mutations that are associated with aggressive types of cancer.
“Afirma is a tool for when FNA isn’t able to tell you what this truly is,” says Ossama Lashin, MD, PhD, a staff Endocrinologist at Cleveland Clinic. “This test offers that exclusion ability to tell us, ‘This is likely benign,’ or, ‘this is likely malignant.’ So rather than saying, ‘Well, this is suspicious. We’ve got to take it out,’ like we used to do in the past, now we can avoid unnecessary surgeries.”
The Afirma Xpression Atlas has been a very useful tool that provides information about specific genetic mutations associated with certain types of thyroid neoplasms. This kind of insight informs clinical decision-making as a management plan is being put together for the patient. If Dr. Lashin encounters a case of recurrent or metastatic or radioiodine refractory thyroid cancer, knowing the type of genetic alteration can guide the treating team to available targeted systemic therapy if the need arises. “That becomes another piece of important information that the care team can use to the advantage of the therapeutic plan,” he explains.
Advertisement
Using ultrasound guidance, three FNA passes are usually performed to collect samples from each nodule in question. Two of the passes are used for cytopathology assessment, and another pass is used for the Afirma Genomic Sequencing Classifier (GSC). The samples are packaged and shipped, and the results typically return in two to four weeks.
“Based on the test results, we can determine the next steps of care — either monitoring or surgery,” explains Dr. Lashin. “But it’s important to remember that every case is different, and if the available cytopathology findings do not support the need for surgery, monitoring of known thyroid nodule(s) and reassessment of risk over the following few years is important. There is always a need to formulate an individualized management and monitoring strategy on a case-by-case basis. Afirma GSC and XA give us more information that we can use to really tailor our treatment plan to each patient.”
Beyond just providing information to the thyroidologist, the findings from the molecular profiling test can also be used to help guide discussions with patients when they’re considering the next steps. “There’s inherent risk in doing partial or total thyroidectomies,” explains Joyce Shin, MD, an endocrine surgeon and the surgical director of the Cleveland Clinic Thyroid Center. “So we always talk to the patients about their surgical options, and it’s very individualized. The extent of surgery depends on the ultrasound findings, Afirma testing results, the patient’s level of anxiety and their past medical, surgical and family history. If cancer is found in half of the resected thyroid, we sometimes have to take the patient back for a second surgery. This means patients will undergo general anesthesia twice, which is not preferable for patients. So a lot of these factors come into play when we have the discussion with patients regarding their surgical options.”
Advertisement
While endocrinologists and endocrine surgeons at Cleveland Clinic recognize molecular profiling as a useful tool, one of the primary challenges is limited awareness of it among other specialties. “Most of the biopsies we perform are done within our Endocrinology and Metabolism Institute, which is unique in that it consists of both endocrinologists and endocrine surgeons,” says Dr. Shin. “However, many patients are being referred by primary care, OB/GYN, of other specialties to get an ultrasound and then possibly a biopsy with radiology. So when they have the biopsy performed without molecular testing and it’s one of these indeterminate nodules, patients will have to come back for another biopsy to include molecular testing. This can be really frustrating for the patient. So we’re trying to help raise awareness among referring physicians from other specialties that this tool exists. Most molecular profiling tools, including Afirma, are covered by insurance, so it is not expensive, and it is now the standard of care.”
Advertisement
Advertisement
Pheochromocytoma case underscores the value in considering atypical presentations
Advocacy group underscores need for multidisciplinary expertise
A reconcilable divorce
A review of the latest evidence about purported side effects
High-volume surgery center can make a difference
Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D
Patients spent less time in the hospital and no tumors were missed
A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications