Falling from standing height should not break bones
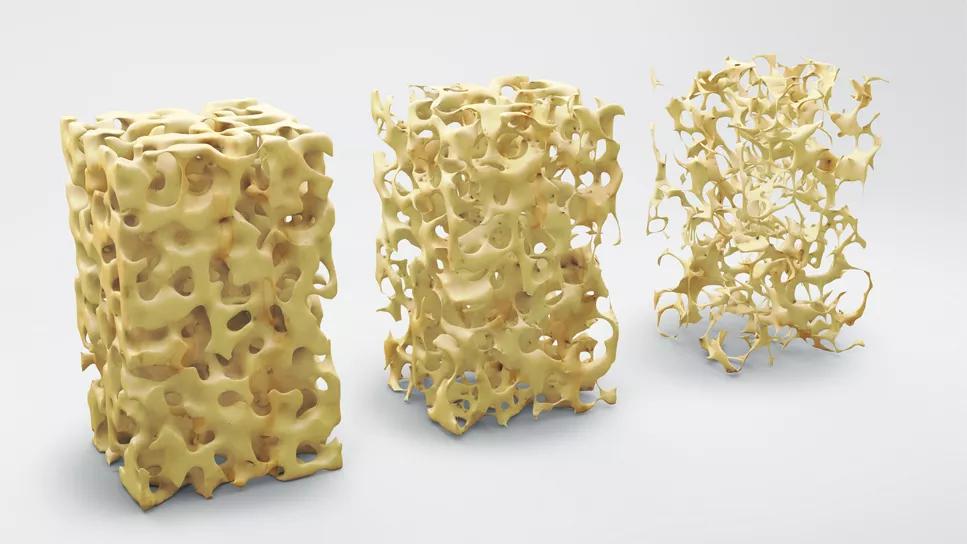
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fb8c70ce-4f9d-4723-b0a1-d5954c9911c5/bone-structure-osteoporosis-667380856)
Illustration of porous bones
Cleveland Clinic endocrinologist Leila Khan, MD, has a family story that illustrates a common misperception about bone fragility.
In 1990, Dr. Khan’s 70-year-old grandmother fell after being pushed by her cousin, a toddler, while babysitting. Her grandmother, who previously was active, broke her hip and spent months recovering. While she ended up doing her rehab at home and was lucky to return to her prior level of functioning, the explanation was that Dr. Khan’s cousin “caused” the break. In reality, the fall likely would not have happened if Dr. Khan’s grandmother had strong, healthy bones. Instead, she had osteoporosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In 1990, there were no available medications for osteoporosis. There was not much to offer,” says Dr. Khan, Co-Director of the Calcium/Parathyroid Center at Cleveland Clinic’s Endocrinology, Diabetes and Metabolism Institute. “Now we have much better treatment options.”
While treatment for bone fragility has improved, there is still a lag in understanding of the significance of osteoporosis bone breaks in adults. Raising awareness is crucial to timely diagnosis, and treatment can mean the difference between living a healthy, active life or suffering with fracture that can reduce quality of life and even result in premature death.
The most important message, says Dr. Khan, is that adults don’t typically break bones from falling from a standing height. A broken bone is a sign to take action.
“Even if it's icy, even if the floor was wet, it is really abnormal to fracture,” says Dr. Khan. A fracture from standing height “results in a diagnosis of osteoporosis.”
Primary care doctors and clinicians who treat patients with such fractures should be referring them for further screening, but that does not always happen.
“What's common is that the patient goes to Orthopaedics, gets their bone fixed, and then their underlying bone fragility is not evaluated,” says Dr. Khan. “We would like these patients to come to Endocrinology or colleagues in Rheumatology, Women’s Health or Internal Medicine for an evaluation.”
Patients are unlikely to ask for additional testing. “They're tired. They may not know the importance of getting this done,” says Dr. Khan. “They may think, well, it’s just a fracture. But they have other bones that they could also fracture.”
Advertisement
In 2010, an estimated 158 million individuals were at high fracture risk. This figure is expected to double by 2040 because of demographic shifts.1 It is estimated that worldwide, one in three women and one in five men over age 50 will experience osteoporosis fractures in their remaining lifetimes.2
“Understanding family history is critical, because there are genetic risk factors,” says Dr. Khan.
The CDC recommends dual energy X-ray absorptiometry (DEXA) bone density testing for women 65 and older or who are 50 to 65 and have certain health conditions that put them at higher risk. Men age 70 years and older also need testing.
Bone mineral density is measured in grams per centimeter squared. Results for people over 50 are translated into T score, which helps stratify risk. T scores run from 0 into negative numbers; 0 to -1 is normal; -1 to -2.5 confers osteopenia; scores of -2.5 or lower are considered osteoporosis. Understanding the risks allows pharmaceutical treatment and lifestyle changes to begin. That puts patients in a better position to avoid additional fractures and the risks that come with them.
Once bone fragility has been diagnosed, it can be successfully treated with medication and lifestyle changes.
“Patients can take a bisphosphonate tablet, which is an antiresorptive, or they can receive a yearly IV infusion of zoledronic acid or a shot every six months called denosumab,” says Dr. Khan. “Or they can start a medication to build up their bone with a daily shot called teriparatide or abaloparatide, or a monthly shot of romosozumab.”
Advertisement
Medical interventions reduce fracture risk between 30% and 60%, depending on the medication. When Dr. Khan works with patients, she gathers family history information and also emphasizes the importance of fall prevention and exercise.
“Exercise, such as walking or weight lifting, is absolutely critical,” she says. ”The bone is a living organism and when we exercise, we significantly improve bone density. It can make a huge difference in preventing the breakdown of bone.”
Increasing awareness among clinicians is also essential. A quality improvement initiative was recentlystarted to increase bone-density screenings among primary care post-menopausal women who should be having them. Dania Salih Bacha, MD, a Cleveland Clinic internal medicine fellow, worked with colleagues to expand understanding of when and how often to order bone mineral density tests.
Despite the CDC’s age- and risk-dependent screening recommendations, in outpatient settings, DEXA test orders are often overlooked. Unlike mammograms and colonoscopies, timely reminders for repeat bone density screenings were not programmed into patients’ electronic medical records, so Dr. Salih Bacha and her teamintroduced several interventions. They created a flow chart to remind physicians when a patient would be due for a repeat bone scan and created an educational podcast on osteoporosis diagnosis and treatment.
The most effective change, however, was adding a reminder to the health maintenance tab in the EMR.
“For every woman older than 65 years who either did not have a bone scan or was due for a repeat scan, a reminder will pop up that this patient needs a DEXA scan,” says Dr. Salih Bacha. “If osteoporosis is added to her medical history, then by default an alert should come up every two years that she needs a new scan. If the physician believes a patient is at lower risk or higher risk, they can manually adjust that interval.”
Advertisement
Reminders that yield high rates of testing can make a real difference for those who are unaware of their risk.
“This is a silent disease,” says Dr. Khan. “People have no symptoms until they fracture, and when they start fracturing, there could be a cascade of fractures that can really alter the course of their life.”
With medication and lifestyle interventions, patients with low bone density can protect themselves and preserve their good health for years to come.
Advertisement
Advertisement
Proactive bone-health management may reduce morbidity and mortality
Finally, a solution after multiple revision surgeries for delayed bone healing, loose hardware and unrelenting infection
Pheochromocytoma case underscores the value in considering atypical presentations
Advocacy group underscores need for multidisciplinary expertise
A reconcilable divorce
A review of the latest evidence about purported side effects
High-volume surgery center can make a difference
Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D