Number of stent layers correlates with worse outcomes
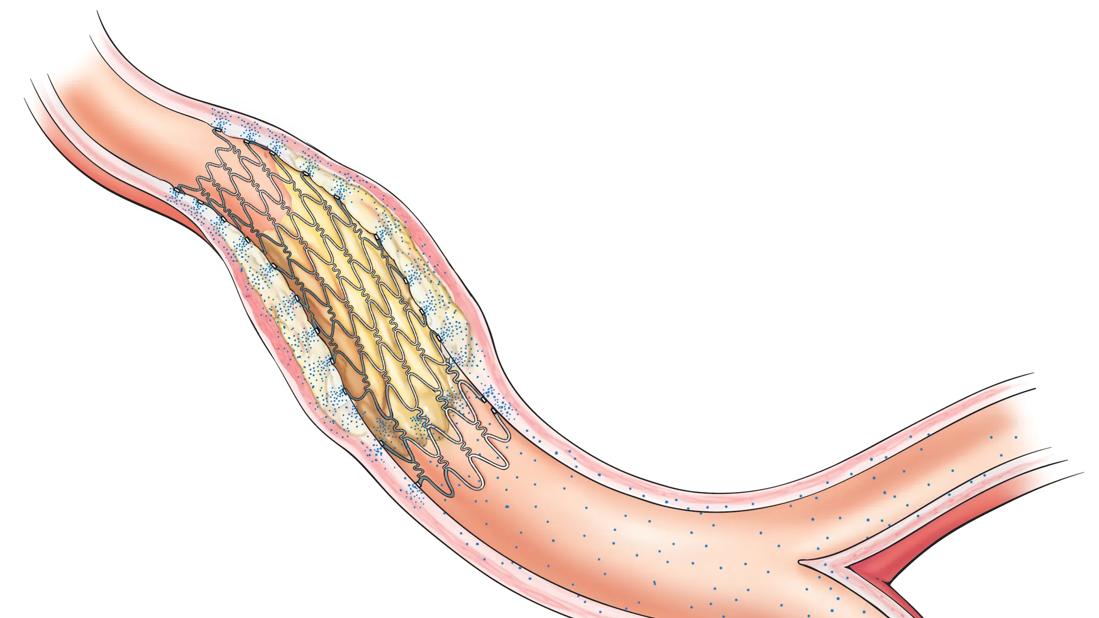
Intracoronary brachytherapy (ICBT) is used at some U.S. centers to treat patients at high risk of coronary stent restenosis. In a new Cleveland Clinic retrospective analysis of patients with recurrent drug-eluting stent (DES) in-stent restenosis, ICBT was associated with target lesion failure in 18% of cases at one year and 46% at three years. Additionally, target lesion failure — i.e., the need to treat the radiated lesion again with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) — was more likely with a higher number of stent layers. The analysis (J Soc Cardiovasc Angiogr Interv. Epub 30 Dec 2022) concluded that ICBT is a safe and feasible option for treating recurrent DES in-stent restenosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Re-blockage within a stent occurs in about 5% to 6% of second-generation DESs at five years, leading to ischemic symptoms requiring further treatment. Recurrence of such in-stent restenosis is even more problematic, with repeat failure rates of 12% to 14% at one year and higher with increasing stent layers.
“In-stent restenosis isn’t particularly common, but it does happen,” says Cleveland Clinic interventional cardiologist Stephen Ellis, MD, the study’s senior author. “It seems that some patients are more prone to this than others, and we don’t yet fully understand why that is.”
Current U.S. guidelines recommend that in-stent restenosis be treated with placement of a second DES. However, if multiple stent layers are already present or if the target vessel isn’t favorable to repeat stenting ― as in cases of small vessel size or bifurcation ― either CABG or ICBT can be considered.
The new data represent the most comprehensive published analysis of outcomes with the use of ICBT ― in which temporarily implanted radiation sources deliver high radiation doses to the lesion ― in this setting. The procedure, which requires close collaboration between cardiology and radiation oncology teams, is currently performed at a few dozen U.S. centers. These include Cleveland Clinic, which maintains one of the highest volumes.
“Treatment options for DES in-stent restenosis are limited,” Dr. Ellis notes. “Balloon angioplasty alone doesn’t do a very good job. Restenting after a couple of blockages adds more metal and often sets the patient up for reblockages that are even harder to treat successfully. We don’t yet have access to drug-eluting balloons. There are medications, but if the patient is highly symptomatic, sometimes they don’t work.”
Advertisement
In contrast to the U.S., European guidelines recommend using a second-generation DES or a drug-coated balloon ― with preference for the latter ― for patients who already have at least two stent layers. Brachytherapy isn’t currently available in Europe, while drug-coated balloons are not yet approved for commercial use in the United States, although that is likely to change within the next year, Dr. Ellis says.
While bypass surgery is certainly an option, many patients don’t want it due to its invasiveness. “If there’s an alternative that may buy them a few years, some are willing to take that option,” Dr. Ellis explains. “In this analysis, we were trying to better understand how to predict outcomes for these patients.”
The study evaluated 330 consecutive patients treated with ICBT for DES in-stent restenosis at Cleveland Clinic from 2010 to 2021; 70% were male and the mean age was 66 years. Nearly two-thirds had already undergone bypass surgery, and 89% had received at least two stent layers at the treated site.
Patients were treated with balloon angioplasty, laser atherectomy and/or rotational atherectomy, followed by ICBT doses of 23-25Gy. “This is higher than the typical 18.4-23Gy range used at other centers,” Dr. Ellis notes.
Although data are scarce, it appears that a higher radiation dose may produce better short-term results by improving suppression of neointimal proliferation. “While further confirmatory data are needed, I suggest working with radiation oncology to see if they want to consider going to a higher dose,” Dr. Ellis advises clinicians at centers that use ICBT.
Advertisement
The target lesion failure rates were 17.7% at one year and 45.8% at three years. All-cause mortality rose from 6.2% to 21.5% and cardiac mortality from 3.6% to 12.3%, respectively, at those time points.
The number of stent layers correlated significantly with target lesion failure at three years, with rates of 33.3%, 47.0%, and 60.2% for one, two, and three or more stents, respectively (P = 0.045).
“The cardiology community appears to be coming to embrace the idea that two layers should really be the maximum,” Dr. Ellis observes. “I think the practice of simply layering one stent over another and then another and hoping things turn out well is not a good idea.”
Lower radiation dose and restenosis within a year of the previous PCI were correlated with target lesion failure at one year (P = 0.035 and P = 0.044, respectively), but not at three years.
Other examined factors — including diabetes, repeat ICBT, final percent stenosis and lesion length — were not associated with one- or three-year outcomes.
In addition to Cleveland Clinic’s use of higher radiation doses, Dr. Ellis notes that “we do almost all our stent procedures under the guidance of intravascular imaging with intravascular ultrasound, whereas that’s not the case in many centers. We think our results are improved as a result.”
The Cleveland Clinic team is currently discussing the feasibility of conducting a head-to-head trial of ICBT versus drug-eluting balloons once the latter are available on the U.S. market. Such a trial has not yet been conducted. In the European experience, outcomes with drug-eluting balloons also appear to vary according to the number of stent layers, Dr. Ellis says.
Advertisement
“I have been happy to support Cleveland Clinic’s intracoronary brachytherapy program since I was a fellow, and I am excited about the possibility of a head-to-head comparison between ICBT and drug-eluting balloons,” says study co-investigator and radiation oncologist Jay Ciezki, MD. “Data comparing more contemporary treatments to ICBT are currently lacking.”
Until such data emerge, Dr. Ellis describes brachytherapy as “imperfect but viable. For symptomatic patients in whom bypass is not a good option, I think it’s the best treatment we have right now in the United States.”
“This study is important in furthering our understanding of the role of intracoronary brachytherapy in contemporary PCI patients who have been treated with second-generation drug-eluting stents,” adds co-investigator Laura Young, MD, an interventional cardiologist. “The data suggest that these patients can benefit from brachytherapy for symptom relief. While it is not a perfect solution, having intracoronary brachytherapy in our armamentarium contributes to our ability to provide such comprehensive care.”
Advertisement
Advertisement

An update on the technology from the busiest Gamma Knife center in the Americas

Radiation oncology department finds weekly plan of care meetings have multiple benefits

Daily five-fraction partial breast irradiation (PBI) shows similar acute and late toxicity as every other day PBI
Study offers a foundation for additional research to examine radiation and immune response

A scannable recap of our latest data in these clinical areas

Key themes and insights into the family-caregiver experience

Pediatric specialists unpack new evidence, considerations for care and what’s ahead

In the wake of NOTION-3 findings, a strong argument for physician judgment remains