Collaborative research effort underscores the urgent need for effective second-line therapies in this rare, aggressive cancer
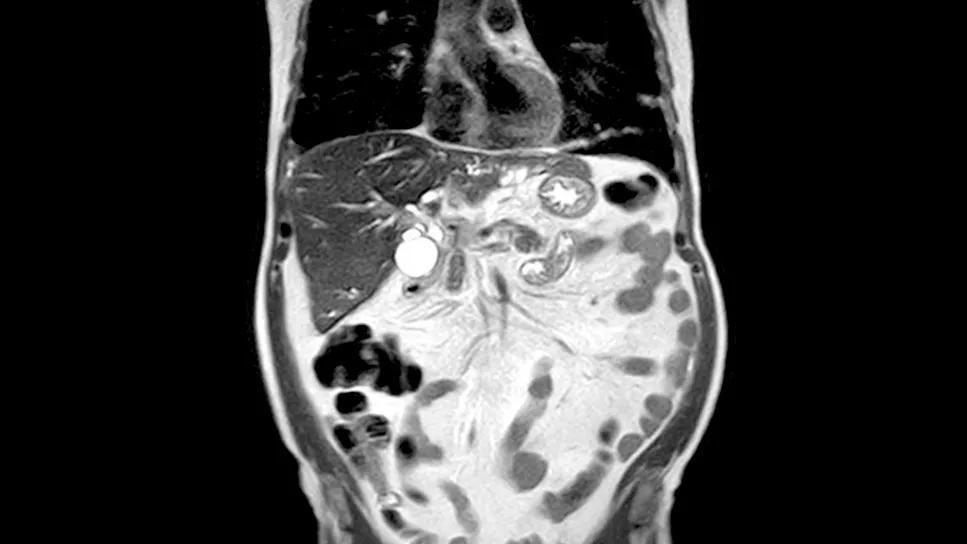
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/56cdf2ed-7e97-40d6-a17a-7144c25a6424/cholangiocarcinoma-a-rare-and-aggressive-cancer-1452991013)
scan showing cholangiocarcinoma
Cholangiocarcinoma—a rare and aggressive cancer arising from the bile ducts—remains a formidable clinical challenge. The options for patients whose disease progresses after initial treatment remain inadequate and largely ineffective. The ECOG-ACRIN EA2187 trial, presented during the 2025 ASCO Annual Meeting, sought to address this critical gap.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We’ve had a pretty clear standard for first-line treatment—typically a combination of chemotherapy and immunotherapy,” notes study author Suneel Kamath, MD, Department of Hematology and Medical Oncology, Cleveland Clinic Cancer Institute. “However, once that stops working, we’ve been left with no real satisfying treatments to give next. The options are few, and the effectiveness is limited. We’re always looking for something better in that second-line space.”
Pevonedistat emerged as a candidate based on promising activity in a previous phase 1 study. The drug works by targeting the NEDD8-activating enzyme, which plays a role in cellular protein degradation. “The mechanism is interesting,” says Dr. Kamath. “Our cells have built-in pathways to trigger death when they’re old or damaged or to repair DNA damage that can randomly occur, but cancer cells hijack those mechanisms to survive. Pevonedistat aims to block the NEDD8-activating enzyme, essentially making the cancer cells more vulnerable to DNA damage and tumor cell death.”
The EA2187 trial was designed to test pevonedistat both as a monotherapy and in combination with the chemotherapy backbone of carboplatin and paclitaxel. This randomized, non-comparative, phase 2 study enrolled 40 patients with unresectable or metastatic intrahepatic cholangiocarcinoma (ICC) who had experienced progression following gemcitabine-based therapy. Participants were randomized to receive either pevonedistat monotherapy (Arm A) or pevonedistat combined with carboplatin and paclitaxel (Arm B).
Advertisement
The trial employed a two-stage minimax design, targeting an objective response rate (ORR) of 30%. The primary endpoint was ORR per RECIST v1.1. Secondary endpoints included clinical benefit rate (CBR), progression-free survival (PFS), overall survival (OS) and safety. Toxicities were graded using CTCAE v5.0.
Of the 40 patients enrolled in the study, 34 were eligible and underwent treatment (17 per arm). The median follow-up was 29.3 months. Unfortunately, no objective responses were observed in either treatment arm.
Stable disease was reported in 35.3% of patients (11.8% Arm A, 58.8% Arm B). One patient in the combination group experienced stable disease lasting more than 24 weeks, translating to a modest clinical benefit rate of 5.9%. Median progression-free survival was 1.54 months for Arm A and 2.92 months for Arm B. Median overall survival was 4.80 months and 6.54 months, respectively.
In terms of safety, grade 3 or higher adverse events were significantly more frequent among patients in the combination cohort (70.6%) than in those who received pevonedistat alone (17.6%). These toxicities included fatigue, cytopenias, febrile neutropenia and nausea/vomiting, among others. Two treatment-related deaths occurred in the combination arm, due to sepsis and colonic perforation.
Unfortunately, the study results did not support further development of pevonedistat for this indication, according to Dr. Kamath. “These findings reflect how difficult this disease is to treat,” he says. “In many other cancers, you can still get responses with second- and third-line therapies. But in cholangiocarcinoma, resistance is often already high after first-line treatment, and that is what we’re seeing with this trial as well.”
Advertisement
Despite these results, Dr. Kamath emphasized the trial’s significance in other key areas, particularly collaboration and infrastructure for rare disease research. “We brought together several centers that hadn’t traditionally worked together. And even during the COVID pandemic, we accrued 40 patients in a relatively short period of time. That shows what’s possible when there’s alignment and commitment.”
Dr. Kamath also highlighted the value of cooperative groups like ECOG-ACRIN, which rely on federal funding to pursue important lines of inquiry. “Pevonedistat might not be the answer here, but the infrastructure allowed us to test it rigorously and quickly.”
While pevonedistat won’t move forward in this setting, the study provides a valuable blueprint for how to approach research in rare cancers like ICC. It also underscores the pressing need to develop second-line therapies that are both effective and tolerable.
“This trial is a reminder of how high the bar still is for treating cholangiocarcinoma, especially when the first-line fails,” concludes Dr. Kamath. “But it’s also proof that we can run well-structured, meaningful studies—even in rare diseases—through strong collaboration and public investment.”
Advertisement
Advertisement
Combining RFA with stenting improves survival rates, reduces post-ERCP complications
A call for awareness about the importance of genomic testing
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates