Case Report and Images of Note
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Peutz-Jeghers Syndrome (PJS) is a hereditary cancer syndrome characterized by benign hamartomatous, primarily gastrointestinal (GI), polyps; muco-cutaneous pigmentation; and a high predisposition to many intestinal and extra-intestinal cancers.
PJS is caused by a mutation of the STK11/LKB1 gene, which normally functions as a tumor suppressor and cell growth regulator. Mutation disrupts the gene’s ability to curtail cell division, leading to polyps and cancer.
Approximately half of cases are inherited from a parent; the remainder occur in patients with no family history of PJS and appear to result from a spontaneous mutation. A patient with PJS has a 50% chance of passing the condition on to their offspring. PJS is relatively rare, affecting one in 25,000 to 300,000 live births of all ethnicities.
Polyps typically occur beginning in childhood in the small intestine but also manifest throughout the intestinal tract and outside the intestinal tract in the renal pelvis, lungs, gall bladder, nasal passages, urinary bladder and ureters. Hyperpigmentation — dark blue or brown macules — on the border of the lips and inside the mouth are a tip-off to the diagnosis of PJS and appear in childhood. The pigment may lessen in adolescence and adulthood, and can also occur near the eyes and nostrils, in the perianal area and sometimes on the hands and feet.
PJS patients have a 90% lifetime risk of cancer, including colorectal (most common — lifetime risk 39 percent), gastric, pancreatic, lung, breast, uterine, cervical, testicular and ovarian.
Advertisement
Small bowel obstruction resulting from polyps is a common complication, often in childhood, requiring surgical intervention. Regular imaging studies (MRI/MRE or CT/CTE) and endoscopic surveillance and polypectomy of the intestinal tract, beginning in early adolescence, can reduce the likelihood of intestinal complications. Many other organs in PJS patients require special surveillance for potential malignancies.
A 39-year-old Asian female presented to Cleveland Clinic’s Digestive Disease & Surgery Institute for evaluation of recurrent small bowel obstruction (SBO) in the preceding year. She recently had been diagnosed with PJS, with genetic testing showing deletion of exons 2–8 in the STK11 gene.
She had undergone abdominal surgery of unknown type at age 2 years.
Endoscopic evaluation during the previous six months revealed multiple hamartomatous polyps, 0.5–4 cm in size, throughout the stomach, small bowel and colon. Computerized tomographic enterography revealed multiple dilated small bowel loops with scattered foci of intussusception, suspected to be due to hamartomatous polyps, leading to recurrent SBO.
Exploratory laparotomy with surgically assisted enteroscopy to the terminal ileum and removal of clinically significant polyps, i.e., “clean sweep,” was planned.
Intraoperative findings included extensive intra-abdominal adhesions and prior small bowel resection, with an anastomotic stricture 60 cm proximal to the ileocecal valve. Surgical adhesiolysis and small bowel resection was performed, along with endoscopic removal of more than 30 polyps >10 cm in size and more than 35 polyps 2–10 cm in size.
Advertisement
These unique intraoperative endoscopic images, obtained with the patient’s consent and originally published in the American Journal of Gastroenterology, depict:

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/65cac6ef-93ff-42b4-bd7a-e3feb390e04d/Image-A_jpg)
Figure 1a — The transilluminated jejunum and ileum.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8e707d4d-242b-4303-b794-a5d6943bc30d/Image-B_jpg)
Figure 1b — Large polyps in the jejunum and ileum.
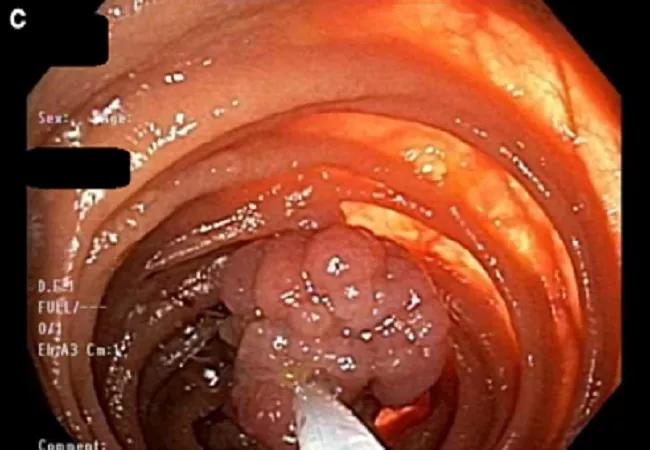
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c9da4ac6-523b-4498-a296-98274587c566/Image-C_jpg)
Figure 1c — Resection of polyps using hot snares and retrieval with a Roth Net or by enterotomy.
The patient has done well after surgery and returns for routine procedures recommended for patients with PJS.
We are fortunate that innovations in small bowel imaging such as video capsule endoscopy and MRI enterography are available to screen for small bowel polyps, and that advances in endoscopic equipment such as balloon enteroscopy are available to remove polyps deep in the small intestine, avoiding the need for emergency surgery in PJS patients.
Dr. Burke is Vice Chair of Cleveland Clinic’s Department of Gastroenterology and Hepatology and Section Head of Polyposis in the Sanford R. Weiss, MD, Center for Hereditary Colorectal Neoplasia.
Adapted from Rao BB, Kalady MF, Burke CA. Intraoperative Enteroscopy in Peutz-Jeghers Syndrome. Am J Gastroenterol. 2018 Jun;113(6):799.
Intraoperative images © The American College of Gastroenterology 2018. Used with permission.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches