Pilot Study at Cleveland Clinic is Testing Feasibility and Biodistribution
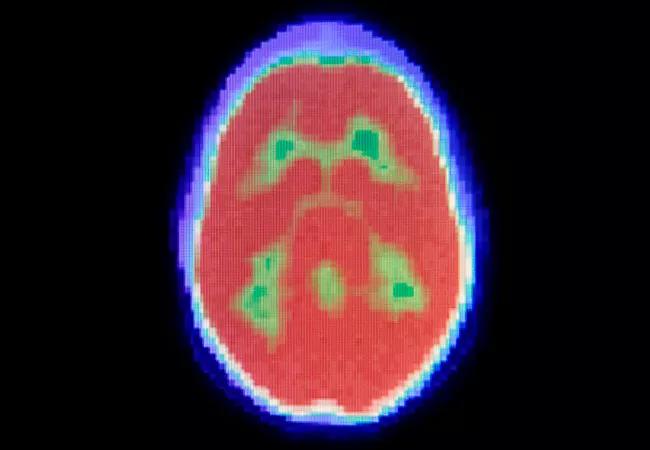
The feasibility of using 18F-clofarabine as a diagnostic imaging tracer to measure deoxycytidine kinase (DCK) activity in solid tumors and their metastases is being explored in a pilot study being conducted at Cleveland Clinic. Currently, no positron emission tomography (PET) imaging agent in routine use measures the activity and function of tumor intrinsic pyrimidine metabolism, which is critical to determine the clinical activity of several mainstay cancer therapies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The purpose of the pilot study is to evaluate feasibility and the biodistribution of clofarabine as a radiotracer,” says Omar Mian, MD, PhD, radiation oncologist at Cleveland Clinic and principal investigator of the pilot study. “We’re asking, is the radiotracer being taken up by tumors and lighting them up without causing significant side effects?”
Clofarabine is a purine nucleoside analogue approved by the U.S. Food and Drug Administration for the treatment of relapsed or refractory pediatric acute lymphoblastic leukemia. Like several other nucleoside analogues, clofarabine must be converted to its active form by DCK. The 18F-labeled clofarabine is chemically identical to the original clofarabine drug molecule, but its stable fluorine atom is isotopically substituted by its radioisotope 18F.
Though the initial pilot will evaluate feasibility and safety, ultimately, the investigators’ goal is to determine whether PET imaging using microdoses of 18F-clofarabine can localize a patient’s cancer and predict responsiveness to DCK-dependent anticancer drugs such as gemcitabine, says Dr. Mian.
“Clofarabine is enriched in tumor cells that upregulate DCK,” Dr. Mian says. “Response to a number of standard chemotherapies such as gemcitabine, fluorouracil and cytarabine depends on expression levels of DCK that would increase the tumor’s uptake of clofarabine as a radiotracer.”
Ruling out candidates for DCK-dependent chemotherapies when tumors have no uptake of 18F-clofarabine would avoid exposing patients to toxicities while permitting selection of potentially more effective alternate first-line therapies, rather than waiting for failure of standard therapies, says co-investigator Zhenghong Lee, PhD, professor at Case Western Reserve University. The imaging agent is applied at a subtherapeutic dose to probe DCK status. “If the enzyme is active, it’s more likely that the cancer will respond to standard treatment because it is of the same family as the radiotracer,” he says.
Advertisement
Planned enrollment into the pilot study is 15 patients with newly diagnosed or relapsed metastatic epithelial solid tumors. Patients will be required to have an Eastern Cooperative Oncology Group Performance Score of 0 or 1 and adequate bone marrow, renal and hepatic function. Pregnancy, lactation, brain metastases and significant comorbidities are key exclusion criteria. All patients will first be seen by their treating physician and then referred to the study coordinator for eligibility screening, enrollment and registration.
“We expect potential toxicities to be absent or minimal, given the microdoses of the imaging agent administered,” says Dr. Mian. “Fifteen patients will not be enough to segregate responders from nonresponders to DCK-dependent therapies, although we may get a signal in that direction. We’re limiting the pilot study to patients with known metastatic cancers to allow comparisons with conventional imaging in that population.”
As part of the study, enrolled patients will receive a baseline 18F-clofarabine PET/computed tomography (CT) evaluation. They will undergo routine follow-up and treatment for their cancer throughout the study period, including repeat 18F-clofarabine PET/CT scans according to standard-of-care follow-up imaging, which is expected between about one and four months after the initial imaging scan. The study will monitor patients for side effects that occur in the 24 hours after their PET/CT scan.
The PET imaging agent will be administered within 28 days of enrollment. Participants are expected to be on the study for up to one year to allow for a variable standard-of-care interval between screening, initial imaging and follow-up imaging.
Advertisement
“Patients would want to consider entering this study because it could help personalize cancer treatments in the future, matching cancers to the best drugs to treat them,” says co-investigator Yogen Saunthararajah, MD, staff and professor of medicine, Department of Translational Hematology and Oncology Research, Cleveland Clinic Taussig Cancer Institute. “Patients will receive a relatively low-risk intervention that could help us better understand and treat cancers on an individual basis.”
Advertisement
Advertisement

Offers a new option for patients 60 and older with relapsed/refractory disease

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Key themes and insights into the family-caregiver experience

Pediatric specialists unpack new evidence, considerations for care and what’s ahead

Discussing research into improving CAR T-cell therapy efficacy

Blinatumomab plus chemotherapy improves overall survival and relapse-free survival over chemotherapy alone

Nurses find unique challenges, profound rewards when managing children with cancer