Offers a new option for patients 60 and older with relapsed/refractory disease
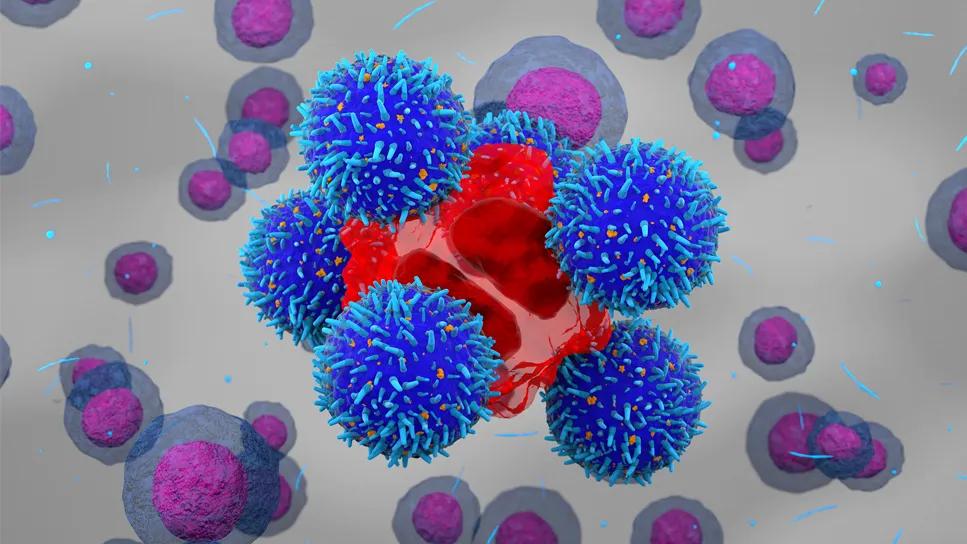
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2a1d2ee5-1abd-4944-8d6e-0186c9e604c9/brexucabtagene-autoleucel-b-cell-1633114212)
CAR T-cell therapy
Chimeric antigen receptor (CAR) T-cell therapy offers an effective new option for patients with relapsed/refractory B-cell acute lymphoblastic leukemia (B-ALL). However, CAR T-cell therapy is also associated with serious toxicities: cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These can be major issues, particularly for B-ALL patients aged 60 and older. Data on the safety and efficacy of the CAR T-cell therapy for B-ALL, Brexucabtagene Autoleucel (brexu-cel), in older patients is limited, which prompted a retrospective multicenter data analysis. Cleveland Clinic participated in this study, which was presented at the annual American Society of Hematology (ASH) meeting in December.
“There is a second peak of ALL cases in older patients (60 years of age and older), most of whom have B-cell disease. For older patients with relapsed/refractory disease, traditionally, the prognosis has been poor,” says study researcher Anjali Advani, MD, a clinician in the Department of Hematology and Medical Oncology at Cleveland Clinic Cancer Institute.
Brexu-cel was the first FDA-approved CD-19-directed CAR T-cell therapy for B-ALL. CAR T-cell therapy uses chimeric antigen receptors (CARs) to engineer T cells to recognize and destroy specific types of cancer. Brexu-cel was approved based on results from the international, multicenter ZUMA-3 trial: of the 71 adult patients over 18 with relapsed/refractory B-ALL who were treated with brexu-cel, 39 patients (71%) had complete remission (CR) or complete remission with incomplete hematological recovery, with 31 (56%) patients reaching complete remission at the median follow-up of 16.4 months.
“The overall response rates were high given that these were very sick patients. However, the number of older patients treated on ZUMA-3 was small,” says Dr. Advani.
Advertisement
To learn more about this patient population, study researchers evaluated data from the Real-World Outcomes Collaborative for CAR T in Adult ALL (ROCCA) consortium database from 30 U.S.-based institutions, the largest study to date. “When older patients asked about outcomes and toxicity, we didn’t have good data to share. The ROCCA database includes patients treated outside of a trial. That real-world experience is needed to inform care,” says Dr. Advani.
Of the 280 brexu-cel recipients in the ROCCA database, 73 (26%) were 60 and older, of which 58 (79%) were 60-69 years old and 15 (21%) were 70 and older. The patients were heavily pretreated with a median of three prior lines of therapy, which included allogeneic hematopoietic stem-cell transplantation (HSCT) (38%), inotuzumab ozogamicin (41%) and blinatumomab (62%). The latter two drugs are FDA approved for relapsed B-ALL.
Prior to apheresis, 33 patients (45%) had active disease, 34 (47%) were in CR (of whom 14 were MRD-negative) and 6 had unknown disease status. Following brexu-cel treatment, 43 (59%) achieved MRD-negative CR, 20 (27%) had MRD + or CR with unknown [NOTE: line spacing needs to be fixed]MRD status, 6 (8%) had refractory disease and five had no disease evaluation available.
The objective response rate (ORR) was similar between patients aged 60-69 and 70 and older (MRD-negative CR rate: 58% vs 61%, response rate to brexu-cel: 9% vs 6%) and was comparable to patients 60 or younger (MRD-negative CR 66%; response rate 9%).
Advertisement
Regarding toxicities, the rate of all grade ICANS was higher in patients 70 and older (77%) than in patients aged 60-69 (47%) or 60 and younger (49%), with grade 1-2 ICANS occurring at a significantly higher rate in patients 70 and older (44% vs. 20% in patients aged 60-69 and 20% in patients 60 and younger). The opposite was true of rates of CRS, which were similar across age groups (80-84%).
With a median follow-up of 332 days from infusion, patients 60 and older had a median progression-free survival (PFS) of 395 days compared to 547 days in patients younger than 60. Median PFS was lower in the over 70 group (231 days) compared to 677 in the 60-69 cohort.
Median overall survival (OS) was not reached in any of the age groups, and there was no statistically significant difference in 12-month OS (61% in the 70 and older group vs. 69% in the 60-69 cohort vs. 73% in the 60 and younger group).
“The most significant finding is that brexu-cel can be used in older B-ALL patients; the risk of toxicities is higher but manageable. It opens up another option for these patients. However, progression-free survival is still low; we are collecting more data in this population to see if we can improve that,” says Dr. Advani.
CAR T-cell therapy is an active area of drug development: a new CD-19-targeting CAR T-cell therapy for relapsed/refractory B-ALL called obecabtagene autoleucel (obe-cel) has shown promising results in clinical trials and was recently FDA approved. “It has fewer toxicities and may be a better option for older patients,” says Dr. Advani.
Advertisement
Advertisement
Pilot Study at Cleveland Clinic is Testing Feasibility and Biodistribution
Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists
Age alone should not rule out patients from potentially curative treatment
Early results show patients experiencing deep and complete response
Discussing research into improving CAR T-cell therapy efficacy
Higher type 2 immunity observed in persistent CAR T cells
Blinatumomab plus chemotherapy improves overall survival and relapse-free survival over chemotherapy alone
Real-world study shows high response rates that are durable with commercial lisocabtagene maraleucel