Positioning the technology in the current therapeutic landscape
Despite interest and research in the 1990s and early 2000s, brachytherapy as a treatment option for brain tumors fell by the wayside over the past two decades, given concerns about radiation necrosis and an inability to control radiation dosages effectively. As brachytherapy was falling out of favor, Gamma Knife® stereotactic radiosurgery began revolutionizing the treatment of brain tumors and has been a mainstay of successful treatment at Cleveland Clinic for nearly 25 years.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
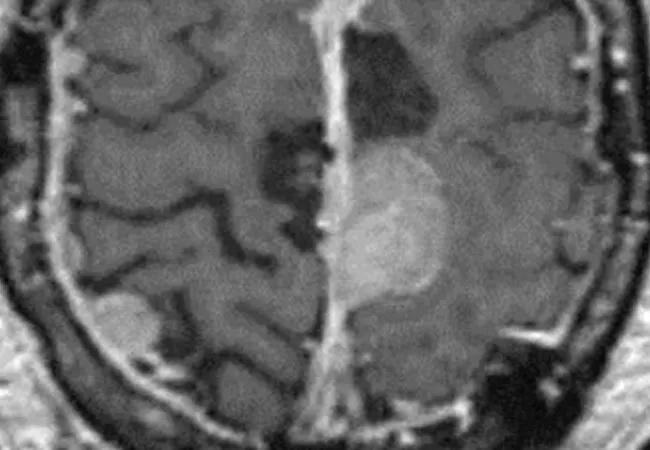
Now interest in brachytherapy in this setting has revived with the recent FDA-clearance of a more targeted form of brain tumor brachytherapy, GammaTile® Therapy. In the following Q&A, Samuel Chao, MD, staff in the Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center in Cleveland Clinic’s Neurological Institute, and Gene Barnett, MD, MBA, director of that center, discuss how this permanent Cs-131 brachytherapy fits into the current therapeutic landscape.
Dr. Chao: GammaTile addresses many of the issues that caused brachytherapy to fall out of favor in the treatment of brain tumors. We used to see issues with excess radiation and injury in some areas where the brachytherapy seeds were placed and, conversely, an insufficient amount of radiation reaching other areas, causing tumor persistence.
GammaTile embeds the seeds in a collagen-based device, so we don’t see the excess radiation and radiation necrosis from direct seed-to-brain contact. It utilizes Cesium-131 and delivers the radiation dose within a few millimeters of the operative bed, so the dose is higher and more targeted than fractionated external beam radiation therapy, which is the current standard of treatment. This is helpful when prior radiation has been delivered to that region of the brain.
Dr. Chao: I think there are a lot of possibilities for reintroducing brachytherapy into the therapeutic landscape for brain tumors in a safer way. As an academic medical center with a robust clinical trial program, we are fortunate to offer our patients the most effective treatments available, and GammaTile is an additional beneficial modality that allows us greater control of radiation dosage. Our colleagues at Cleveland Clinic Florida have recently incorporated the technology into their treatment protocols for patients with refractory disease.
Advertisement
Dr. Barnett: GammaTile can be used anytime surgery is being performed on our brain tumor patients and is a helpful tool for our patients with refractory disease. As we await class 1 evidence to establish the benefits of GammaTile, we are cautiously incorporating it into our practice.
Dr. Barnett: One of the main issues we see is that use of GammaTile may impact patients’ eligibility for clinical trials should they need them in the future. We expect this to be resolved over time, but right now it is a barrier.
Dr. Chao: At Cleveland Clinic, we are fortunate to have highly skilled neurosurgeons and radiation oncologists who push the limits of what we can do with radiosurgery. We were among the first centers to use Gamma Knife, which is one of the best devices for radiosurgery for brain tumors, and we’re a leader in providing Gamma Knife education to other physicians and physicists. This wealth of experience limits our need to use a therapy like GammaTile, except in cases of the most refractory disease.
Dr. Barnett: Patients most likely to benefit include those with recurrent meningiomas who have already undergone multiple rounds of radiosurgery, or those with gliomas who have exhausted all other treatment options.
Dr. Chao: Because most systemic agents do not work on meningiomas, meningioma patients are limited to radiation and surgery as their only treatment options. But these tumors may recur, and once patients have exhausted external beam radiation therapy, radiosurgery and surgery options, and if they are ineligible for clinical trials, we are glad to have GammaTile as an additional modality for them. It allows us to spare sensitive brain structures and limit toxicity in the setting of multiple retreatments with radiation.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient