Total pelvic exenteration is often curative today
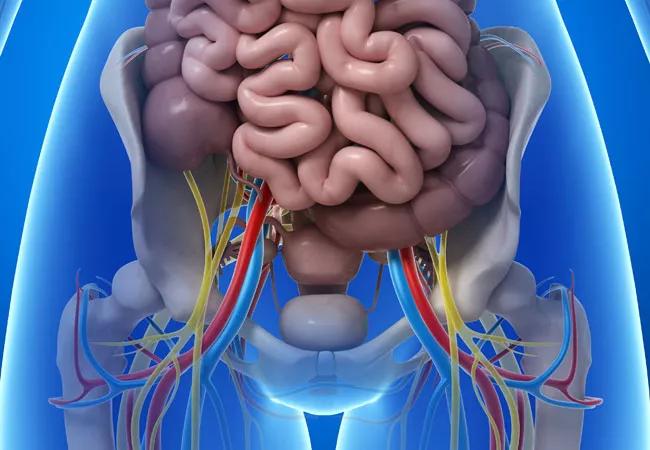
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/45cadb61-07a1-4cf1-9f74-43b05685e923/18-DDI-389-pelvicExenteration_jpg)
18-DDI-389-pelvicExenteration
Total pelvic exenteration (TPE) is an extensive cancer-removal operation that is fortunately not often required. But Cleveland Clinic’s surgeons tackle the procedure a few times a month, assisted by a multidisciplinary team of specialists who each contribute in important ways to the patient’s ultimate ability to proceed with their post-surgical lives.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In women, the procedure involves removal of most or all the pelvic viscera — bladder, uterus, cervix, vagina, rectum, anus and external genitalia. It’s reserved for patients with recurrent gynecologic, bladder or rectal cancer who have already undergone surgery, chemotherapy and radiation. Depending on the location of the cancer, in some cases the bladder or rectum may be spared.
Historically, TPE dates back to the 1940s, when it was used primarily as a palliative treatment for gynecologic cancers. Today, it is often curative. Either way, the procedure and its reconstructive aftermath can dramatically alter patients’ physical and emotional well-being.
“It’s extreme, but if you have a young woman with a recurrent cancer, it’s not a bad option if otherwise she would die,” says Robert DeBernardo, MD, Director of Cleveland Clinic’s Peritoneal Surface Malignancy Program.
Advances in recent decades in surgical and reconstructive approaches have allowed for greater use of TPE in rectal cancer in both women and men as well, says colorectal surgeon Michael A. Valente, DO.
“We’ve become better at it and we’re doing it more, with a big team of experts,” Dr. Valente says. “It’s a life-altering operation, but with overall good success in curing patients and getting them back to normal life.”
Members of Cleveland Clinic’s team involved in TPE and subsequent reconstruction include medical oncologists, gynecologic oncologists, colorectal surgeons, urologists, radiation oncologists, plastic surgeons, pain management specialists, ostomy and enterostomal specialist nurses, and psychosocial support specialists.
Advertisement
The team’s experience also equips them to handle any post-surgical complications, Dr. Valente says. “Here at Cleveland Clinic, we’ve seen every complication. That’s important since there’s not a ton of literature to drive us.”
Advances such as greater application of intraoperative radiation and improvements in anesthesia and transfusions have all contributed to better outcomes.
While laparoscopic and robotic surgical approaches are sometimes used for TPE, neither Dr. DeBernardo nor Dr. Valente consider them to be particularly advantageous and rarely use them. “Since these are such long, radical surgeries, robotic surgery doesn’t typically translate to better cancer outcomes or recovery,” Dr. DeBernardo notes.
Indeed, Dr. Valente says that for TPE, “the vast majority are performed with an old-fashioned open approach because of the complexity of the operation. The ability to get every piece of cancer out of the patient is the most important thing, not how you do the operation.”
Major progress has been made in vaginal reconstruction, such as the use of vertically oriented rectus abdominus myocutaneous (VRAM) flap grafts in the pelvis to minimize post-surgical complications.
In addition, the development of more cosmetically and personally acceptable alternatives to traditional colostomy and urostomy devices has contributed significantly to patient satisfaction.
“We can make continent bladders now so that people can catheterize the pouches and not have to wear appliances. The idea is to create an internal pouch as a reservoir for the urine,” Dr. DeBernardo says. “They’ve been around for years, but we’ve gotten better and better at them.”
Advertisement
He adds, “We now have fancy stapling devices, so we’re not suturing everything together. Outcomes are better, and quicker.”
And, while many TPE patients will still require external colostomies and urostomies, in some cases the one stoma can be combined into two conduits, a so-called “wet colostomy,” so that at least the patient doesn’t need to wear two separate bags.
Addressing the physical and psychological aftermaths of surgery are critical to patient quality of life going forward.
Surgeons need to give patients reasonable expectations, Dr. DeBernardo says. “My patients who are happiest with these operations are those whom I’ve prepared ahead of time on issues such as sexual function and continence. To have that conversation before surgery is extremely important to set expectations and also to have informed consent for decisions that must be made in the OR.”
Sexual function in particular is a crucial topic that surgeons often don’t address and that patients may be reluctant to mention, Dr. DeBernardo notes. “How do you feel sexy with a stoma? There’s a lot of anxiety.”
He sees room for improvement in his profession. “Surgeons like to fix things. We’re very matter-of-fact,” he says. “We don’t have as much of the communication skills. But that’s important, especially if you’re doing an operation that’s going to change someone’s life.”
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years