Helping to ensure optimal outcomes
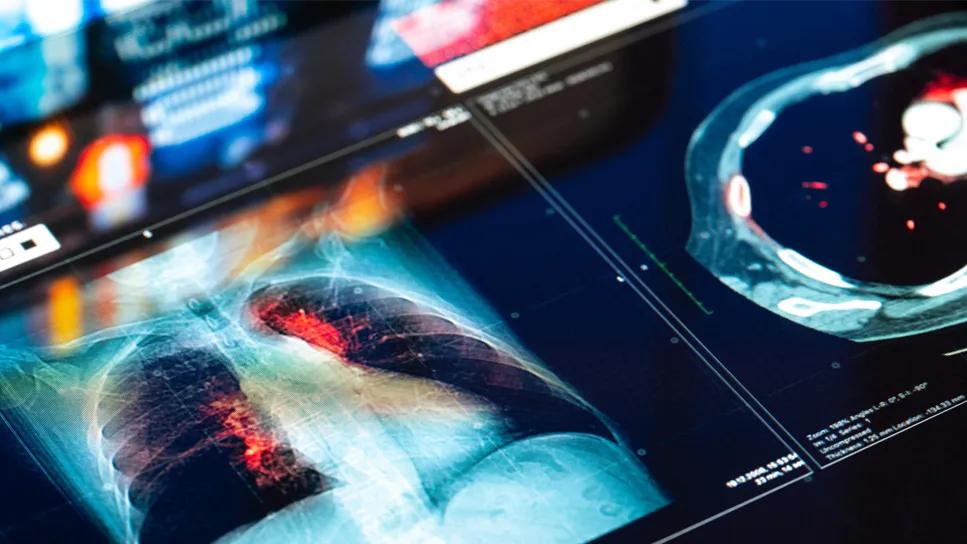
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1f4a92e9-8038-4974-915e-43e2ec48c8c1/lung-transplant-preparation-for-geriatric-1302877802)
Human lungs
As the number of geriatric patients needing lung transplants rises in the United States due to the increasing prevalence of interstitial pulmonary fibrosis, Cleveland Clinic has identified a need to evaluate and better prepare older patients for these surgical procedures to optimize outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The population of the United States is aging, and we are performing more lung transplants in older adults. As a result, we are seeing more complications specific to this age group, including postoperative delirium,” says Marie Budev, DO, MHA, Medical Director of the Cleveland Clinic Lung Transplant Program. “To improve outcomes, we are focusing on factors that can be modified or reversed with the help of our geriatric colleagues. Essentially, we are seeing the birth of a new field of medicine — geriatric transplantation.”
Patients are selected for lung transplant after undergoing a rigorous preoperative workup from head to toe that can take weeks to months to complete, explains Dr. Budev. During this process, these patients are seen by a multidisciplinary team consisting of specialists from pulmonary medicine, cardiology, immunology, surgery, psychiatry, social work and, in the case of older adults, geriatrics. The team meets weekly for approximately 90 minutes to review the status of prospective surgical candidates.
By virtue of being older, geriatric patients have more comorbidities, such as vascular disease, coronary artery disease, neurocognitive dysfunction and underlying malignancies that can lead to poor outcomes after transplant, notes Dr. Budev. “The geriatric physicians perform a battery of neurocognitive assessments and tests for frailty in this population,” she says. “If these issues are found, patients are not excluded from transplant, but rather clinicians may be able to work with them to ‘pre-rehabilitate’ and address reversible or modifiable factors to help better prepare them for transplant.”
Advertisement
According to Luke Kim, MD, a member of the Inpatient Geriatric Consultation Staff, “Although patients over the age of 65 are known to have poorer transplant outcomes than younger patients, we don’t just go by the patient’s chronological age when we are assessing geriatric patients for lung transplant, but also their functional age.”
To evaluate function, Ardeshir Hashmi, MD, Director of the Center for Geriatric Medicine at the Cleveland Clinic and a member of the multidisciplinary lung transplant team, reports that the team begins by evaluating walking/gait speed and hand-grip strength. To further evaluate for frailty, he and his colleagues assess for activities of daily living (ADLs) and instrumental activities of daily living (IDLs) to determine where patients fall on the Clinical Frailty Scale. “Depending on how frail patients’ are,” he says, echoing Dr. Budev’s remarks, “it may be possible to improve their function with physical therapy interventions.”
The geriatrics team also reviews patients’ medication lists, looking for over-the-counter drugs such as sleeping aids and prescription medications such as anticholinergics, benzodiazepines and other sedative hypnotics that may increase the risk of intraoperative physical complications and postoperative confusion, memory impairment and delirium. Anxiety is very common in transplant patients, but specific anxiety medications such as benzodiazepines are potentially inappropriate in the elderly and can delay recovery after transplant surgery.
Advertisement
“We try to adjust the doses early in the screening process and wean older patients off of benzodiazepines entirely if possible in favor of other, safer drugs,” says Dr. Kim. He reports that the team follows the step-by-step slow tapering protocol outlined by the EMPOWER trial, which focused on reduction of inappropriate benzodiazepine prescriptions in patients over the age of 65.
Dr. Hashmi adds, “We discuss patients’ goals for surgery and their expectations, and we make sure they have selected a healthcare proxy to speak for them if they are unable to speak themselves.
“Our goal is to help prospective lung transplant patients as if they are preparing for a major athletic event,” he says. “We want them to be in the best physical and mental shape possible so they have the most optimal outcomes.”
Advertisement
Advertisement
Initiatives focus on the physical and emotional well-being of geriatric patients and their caregivers
Researchers explore the mental and physical benefits of social prescribing
Multidisciplinary approach helps address clinical and psychosocial challenges in geriatric care
Effective screening, advanced treatments can help preserve quality of life
Study suggests inconsistencies in the emergency department evaluation of geriatric patients
Auditory hallucinations lead to unusual diagnosis
How providers can help prevent and address this under-reported form of abuse
How providers can help older adults protect their assets and personal agency