Insights on integrating behavioral health providers into care as the disease progresses
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2243576/13534506)
Patients with Parkinson’s disease can face significant behavioral health challenges stemming from chemical changes to the brain brought on by disease progression and medication interactions. Psychologists and psychiatrists are an important part of the multidisciplinary care team that can address these challenges.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Living with Parkinson’s disease is not easy, and it can wear on patients,” says clinical health psychologist Taylor Rush, PhD, Director of Behavioral Health Services and Interdisciplinary Programs in Cleveland Clinic’s Center for Neurological Restoration. “We want to make sure we can support patients in every way we can throughout the journey.”
In the latest episode of Cleveland Clinic’s Neuro Pathways podcast, Dr. Rush talks about potential behavioral health issues for patients with Parkinson’s disease and how to manage them. She discusses:
Click the podcast player above to listen to the 26-minute episode now, or read on for a short edited excerpt. Check out more Neuro Pathways episodes at clevelandclinic.org/neuropodcast or wherever you get your podcasts.
This activity has been approved for AMA PRA Category 1 Credit™. After listening to the podcast, you can claim your credit here.
Podcast host Glen Stevens, DO, PhD: What advice do you have for clinicians who care for patients with Parkinson’s disease and want to implement some type of behavioral health program into their practice?
Advertisement
Dr. Rush: Listen to your patients and their needs. That sounds pretty obvious, but sometimes when we’re looking at patients, we may see one thing that they really need based on appearance and what we perceive as debilitating when they are actually bothered by things we can’t necessarily see. There can be a lot of non-motor symptoms associated with Parkinson’s — including gastrointestinal symptoms, incontinence issues, visual issues, things like that — that you can’t always detect. And one of those symptoms may actually be bothering a patient more than something observable like tremor.
This makes it important to really ensure that you dig into what it is that they need and what is bothering them, and then to consider whether you see it worsening over time in terms of their sense of control. And it’s important to really make sure they have some sense of what they can do to empower themselves to manage their symptoms.That may amount to making sure that you offer them orders for physical or speech or occupational therapy.
Unfortunately, I have heard patients from other places tell me how they asked for speech therapy or physical therapy and they were told, “But you have Parkinson’s. It’s a neurodegenerative disease. It’s not going to get better.” So they get shut out of being able to learn some of the skills that could be incredibly helpful for them.
It is crucial to recognize that even though these symptoms will get worse over time, we should empower out patients as much as we can to use the tools that may be out there for them. That will help ensure that they have the best quality of life for as long as possible.
Advertisement
Advertisement

Various AR approaches affect symptom frequency and duration differently

Dopamine agonist performs in patients with early stage and advanced disease

Early assessment could affect clinical decision making

Systems genetics approach sets stage for lab testing of simvastatin and other candidate drugs

Study aims to inform an enhanced approach to exercise as medicine

New tool for general neurologists aims to streamline differential diagnosis

When and how a multidisciplinary palliative care clinic can fill unmet needs for this population
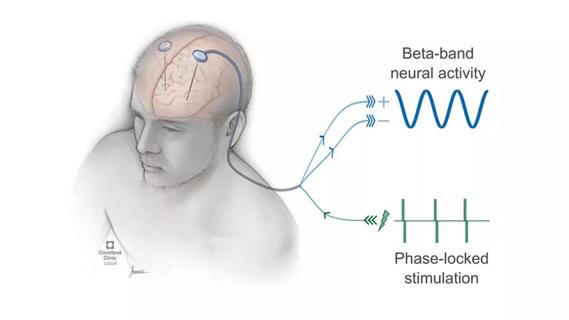
Research project will leverage insights into neural circuits to advance DBS technology