Study combines hormonal therapy with prostatectomy and radiation therapy of bone lesions
Men with newly diagnosed metastatic prostate cancer have long been viewed as incurable. But about eight years ago, Eric Klein, MD, Chairman of the Glickman Urological & Kidney Institute at Cleveland Clinic, encountered a patient that proved otherwise.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“He had presented to us with a high-grade prostate cancer invading adjacent structures and a biopsy-proven lymph node,” says Dr. Klein. “He was treated with hormone therapy for six months and then had his prostate and lymph node removed, followed by radiation to one metastatic site in the bone. Now eight years later, he has no cancer and isn’t taking any medication for it.”
That patient unwittingly may have started a seismic shift in the treatment of metastatic prostate cancer.
“If we can cure one patient with biopsy-proven metastatic prostate cancer in two sites, can we help other patients the same way?” asks Dr. Klein. “And even if we don’t cure them, can we slow down cancer progression so these patients live longer?”
He and a multicenter team of physician-researchers are about to find out.
Cleveland Clinic is participating with other select medical centers recruiting for the clinical trial “Metacure: Multi-arm Multi-modality Therapy for Very High Risk Localized and Low Volume Metastatic Prostatic Adenocarcinoma.”
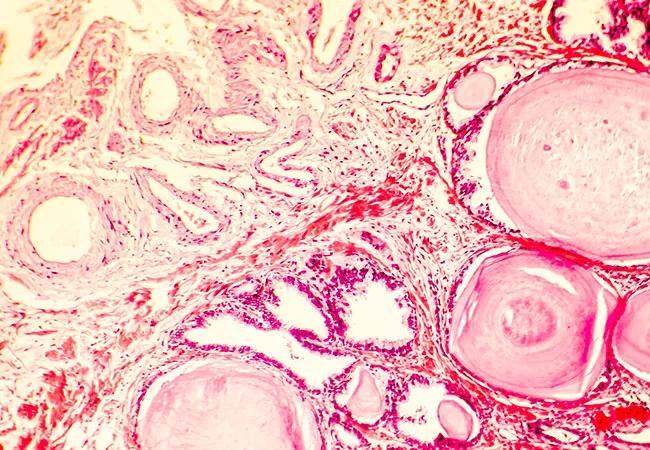
Patients eligible for the Metacure trial are men with newly diagnosed prostate cancer with a limited number of metastases in bone and/or lymph nodes. They begin treatment with systemic hormone therapy and then are randomly assigned to either one or two androgen receptor blockade therapies with apalutamide and/or abiraterone acetate. Patients are monitored for response by prostate-specific antigen test and x-rays. When they reach appropriate response and time points, surgery to remove the prostate and lymph nodes and radiation to bone metastases are performed.
Advertisement
“The goal is to study the long-term clinical benefits, including survival and response rates,” says Shilpa Gupta, MD, a Cleveland Clinic medical oncologist who specializes in genitourinary cancers.
Conventionally, patients with metastatic prostate cancer have been treated with either systemic hormonal therapy or chemotherapy but not treating the primary tumor, she says. However, there is growing evidence — from STAMPEDE and HORRAD trials, for example — that targeting the primary tumor while treating the metastatic disease can improve outcomes. That approach has become common in Europe but hasn’t been widely used in the U.S.
Depending on the results, the robust, prospective Metacure trial may change this U.S. practice.
“This study is a truly multidisciplinary effort,” says Dr. Gupta. “For each trial participant, a urologist must determine if prostatectomy is an option, a radiation oncologist must evaluate the metastatic sites and suitability for radiation therapy, and a medical oncologist must administer the hormonal therapy.”
In addition to potential changes to standard of care, the study may provide new insights into the biology of prostate cancer.
“Since we’ll be looking closely at tumor tissue, we may learn more about why some patients respond to treatment and some don’t,” says Dr. Gupta.
The hypothesis behind this trial is that the best systemic therapy followed by aggressive surgical removal of the prostate and lymph nodes, and aggressive radiation of bone lesions will help some patients. The theory is based on solid science, says Dr. Klein.
Advertisement
Metastases come from the primary tumor in the prostate, he explains. While androgen-deprivation therapy can make metastases regress, it does not sterilize the primary tumor in the prostate — which can continue to give rise to new metastases. It makes sense that both the primary tumor and metastatic lesions need to be addressed in combination, he says.
Omar Mian, MD, PhD, a radiation oncologist at Cleveland Clinic, notes that imaging technologies, like 68Ga-PSMA and Axumin PET, paired with stereotactic radiation, a non-invasive technique that can eliminate prostate cancer in isolated bone lesions and lymph nodes, have enabled medical oncologists to target metastatic spread with greater precision than ever before.
“We have great treatment (radiation or surgery) for local disease and great treatment (hormonal therapy) for metastatic disease,” says Dr. Klein. “Let’s aim these big guns at both targets and see what happens. Let’s see if we can cure some of these men.”
Adding to this, Dr. Mian concurs that the trial signals an exciting shift in prostate cancer medicine. “A new generation of hormone therapies combined with surgery and targeted radiation are extending potentially curative options to patients with low-volume metastatic prostate cancer,” he says.
Not every patient — namely those with a high burden of disease — will be eligible for this approach, adds Dr. Gupta. That’s why this trial is only for oligometastatic disease, where only a few metastatic sites exist, where potential for cure is highest.
Advertisement
“I think that addressing the primary tumor and all the oligometastatic sites with definitive therapy can potentially lead to long-term remission or cure for many men,” says Dr. Gupta. “We’re already doing it in colon cancer. It’s time we try it in prostate cancer as well.”
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient