New study is the first to create and validate a multivariable model in this patient population

A new tool developed and validated by pediatric cardiologists at centers across the U.S. may be used to predict the likelihood of mortality in pediatric patients who are supported by venoarterial (VA) extracorporeal membrane oxygenation (ECMO).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The risk of mortality is high in neonates and children who receive VA-ECMO, an intervention for refractory myocardial failure. The research team behind the risk assessment model, known as Pediatric Survival After Venoarterial ECMO (Pedi-SAVE), says the tool is a game changer in the assessment of multiple concurrent risk factors, allowing physicians to improve parent counseling in an acute care setting.
Bradley Marino, MD, MBA, senior author of the study and Chair of the Department of Pediatric Cardiology at Cleveland Clinic Children’s, says the study addresses a significant gap in the literature. “Prediction models exist for adults, children and neonates supported by respiratory ECMO and for adults supported by cardiac ECMO, but not in the pediatric population supported by cardiac ECMO,” he explains.
Adult and pediatric patients are supported by cardiac ECMO for very different reasons, making it problematic to extrapolate adult data to assess risk in children. VA-ECMO is often utilized to support pediatric patients with myocardial failure, as a rescue intervention for patients who are refractory to CPR , or until they transition to a longer-term therapy, like cardiac transplantation or ventricular assist device placement.
Clinical variables can also greatly vary among the pediatric population, making survival outcomes difficult to predict. “We see a high incidence of congenital heart disease and wide variation in patient size, cardiac anatomy and physiology in children on cardiac VA-ECMO,” Dr. Marino says. “A myriad of factors, including the timing of ECMO initiation, underlying physiology, and the center itself, can influence outcomes in these patients. Such variability warrants a tool to help refine and individualize risk.”
Advertisement
The team developed and validated models by leveraging data from the Extracorporeal Life Support Organization (ELSO) registry. The complete dataset (N = 10,091) included patients supported with VA-ECMO from birth to 18 years with a specific cardiac diagnosis from 2001 to 2015. Of these, 4,996 patients (50%) survived to hospital discharge, the authors report.
Using 2:1 random sampling, they divided the total dataset into two separate groups for modeling (N = 6,727) and validation (N = 3,364). The team then identified variables associated with survival by using multivariable logistic regression and random forest models and created two versions of the Pedi-SAVE score, one that reflected known variables before and after cannulation.
The Pedi-SAVE scores categorized risk into one of five tiers based on patients’ clinical variables. The lowest risk patients have a 65% and 74% chance of survival at discharge using the pre-and post-cannulation models, respectively. The highest risk cohort was much lower with a 33% and 22% likelihood of survival at the same pre-and post-intervention intervals.
“Prior to this study, we knew these patients had about a 50% chance of survival. Now, I can tell parents based on their child’s pre-VA-ECMO descriptors that they have a 33% to 65% chance of survival. And then once they’re on VA-ECMO, based on those variables, we can then project between 22% and 74%.”
The study identified several pre- and post-cannulation demographic and clinical data points that are associated with survival. These include the following:
Advertisement
In addition, post-cannulation variables include lower ECMO pump flows at 24 hours and lack of mechanical, hemorrhagic, infectious, or secondary organ complications (e.g. cardiovascular, neurologic, pulmonary and renal).
Dr. Marino notes that while these individual factors have been previously reported, this is the first validated model to complete a holistic, multifactor analysis for pediatric patients on VA-ECMO.
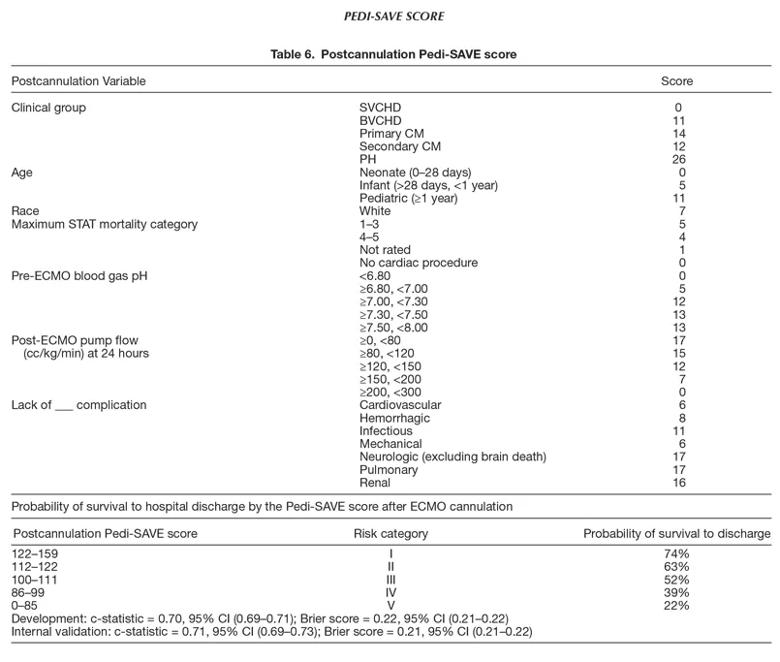
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a3592638-483c-402a-a4b3-ef4af6da00a2/22-CHP-2933557-CQD-Marino-Development-of-a-Model-for-the-Pediatric-Survival_805x263_jpg)
Reproduced with permission from Wolters Kluwer Health, Inc. This table originally appeared in Geisser, Diana L.; Thiagarajan, Ravi R.†,‡; Scholtens, Denise§; Kuang, Alan§; Petito, Lucia C.§; Costello, John M.¶; Monge, Michael C.‖; Di Nardo, Matteo#; Marino, Bradley S.,** Development of a Model for the Pediatric Survival After Veno-Arterial Extracorporeal Membrane Oxygenation Score, ASAIO Journal: February 16, 2022 – Volume – Issue – doi: 10.1097/MAT.0000000000001678
He also says the team was pleasantly surprised by the accuracy of the Pedi-SAVE model but cautions that the data used for the model are only as accurate as what is captured in the ELSO registry. “This is a registry study with over 10,000 patients. There are certain variables relative to the patient that we just don’t have access to but would make the model even stronger,” he notes.
Though the model is not intended for direct individual decision-making, it can be a powerful tool when counseling parents and managing expectations about survival outcomes. “I can sit with a family and discuss their child’s likelihood of survival in a way that wasn’t really possible before, at least not in a way that simultaneously captured different variables,” he says. “We also hope that as survival rates continue to increase, tools like this will help clarify modifiable risk factors to improve longer-term functional outcomes.”
Advertisement
Advertisement

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve