Study shows surgical experience impacts the risk of post-operative stricture formation
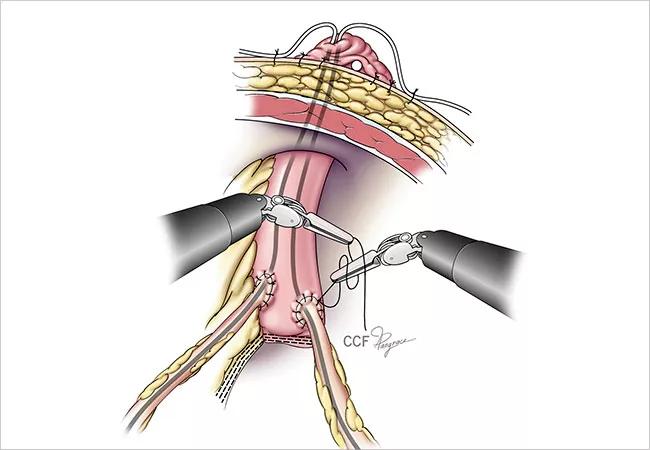
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2d04091a-2897-4689-8163-690b23b72ef6/650x450-Urinary-Diversion_jpg)
650×450-Urinary-Diversion
Performing post-radical cystectomy urinary diversion intracorporeally, with robot assistance, rather than extracorporeally, using an open approach, elevates the risk that patients will develop ureterointestinal anastomotic strictures (UEAS), although that risk declines as surgeons gain experience with the robot-assisted intracorporeal procedure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That’s the conclusion of new Cleveland Clinic research presented at the American Urological Association’s 2019 annual meeting.
The findings from the retrospective single-center study address two key issues in uro-oncological surgery:
The answer to both appears to be yes. The study’s authors say results point to the need to limit ICUD to high-volume urological surgery centers, or to ensure that surgeons performing the procedure have considerable training and experience in robot-assisted urinary diversion, in order to minimize UEAS risk.
“There may be benefits to ICUD, but we have to be realistic about the potential complications and do what we can to prevent them,” says Cleveland Clinic urological surgery fellow Kyle Ericson, MD, the study’s lead author.
Radical cystectomy (RC) with urinary diversion (UD) is the standard of care for muscle-invasive bladder cancer. The conventional open procedure to extirpate the bladder is associated with significant post-operative morbidity. Robot-assisted RC emerged in the early 2000s as a less-invasive alternative. Recent research has shown that the open and robot-assisted RC modalities are comparable in terms of oncological outcomes.
Advertisement
With the rise of robot-assisted RC, some surgeons began to transition from the traditional open, extracorporeal urinary diversion (ECUD) approach to an intracorporeal, robot-assisted procedure — the more technically complex ICUD — to fully leverage the minimally invasive benefits of the robotic platform.
UEAS is a common late complication following RC and UD, with incidence rates ranging from 2.6–13%. Although its exact etiology is unclear, it may result from compromised vascularity due to ureteral damage during manipulation, or improper surgical technique during ureterointestinal dissection and suturing. UEAS is a potential cause of renal dysfunction after RC/UD and significantly impairs patients’ quality of life, as treatment requires surgical intervention or lifelong trans-stomal or percutaneous drainage.
While ICUD and ECUD have similar safety profiles, there is little published evidence comparing the impact of either approach on UEAS incidence. A 2017 retrospective analysis of RC cases performed by a single surgeon suggested a correlation between ICUD and UEAS. The randomized multi-center Robot-assisted Radical Cystectomy versus Open Radical Cystectomy (RAZOR) study found similar UEAS rates (7 and 9%, respectively), but UD in the robot-assisted arm of the trial was exclusively extracorporeal, leaving unaddressed whether the modality of UD would have made a difference in stricture formation.
Utilizing a registry of 968 patients who underwent RC performed by 10 surgeons at Cleveland Clinic between 2011 and 2018, Dr. Ericson and his Glickman Urological & Kidney Institute colleagues sought to compare the incidence of UEAS among open RC, robot-assisted RC with ECUD, and robot-assisted RC with ICUD. They also examined the effect of the surgeon’s experience on the incidence of UEAS following ICUD.
Advertisement
UEAS occurred in 11.3% of the RC patients — 9.3% following ORC, 11.3% after ECUD and 13% after ICUD. With multivariable analysis, ICUD was independently associated with UEAS (hazard ratio 1.64, confidence interval 0.99–2.71, p = 0.05).
Analyzing whether surgeons’ experience impacted the likelihood of UEAS formation, the researchers found that higher sequential ICUD case numbers were independently associated with a reduced risk of UEAS. “Our statistical model showed that an increase in the number of ICUD cases a surgeon performed reduced the risk of stricture,” Dr. Ericson says. Volumes of 75 ICUD cases or less were associated with increased risk of UEAS. For the sole surgeon in the study cohort who performed more than 75 ICUD cases, UEAS incidence decreased from 17.5% to 4.9%.
ECUD was not found to be an independent risk factor for UEAS.
The new research reiterates the need for surgeons to take into account the learning curve for full proficiency in robot-assisted ICUD and its potential impact on ureterointestinal stricture development.
“Comfort with the robotic platform has made ICUD a much more feasible procedure to perform, though it’s still very difficult,” Dr. Ericson says. “The vast majority of urinary diversions following radical cystectomy are still done with an open approach. Early in the learning curve with ICUD, it can be difficult to keep the orientation of the bowel, to make sure the anastomosis is secure, and to keep the orientation of the actual diversion. Gentle tissue-handling without tactile feedback is also a challenge with robotics early in the learning curve. But with experience, we’ve seen that the operative time is shorter with ICUD than ECUD, and that patients may have better outcomes.”
Advertisement
While the study did not attempt to identify the etiology of stricture formation, compromised ureteral vascularity due to increased dissection under magnification and ureteral crush or stretch injuries due to lack of haptic feedback during robotic manipulation are potential factors. To minimize UEAS risk, Dr. Ericson and his colleagues advise that surgeons consistently practice the essential principles of gentle tissue-handling, adequate tissue preservation and spatulation for anastomotic suturing, and a tension-free, liquid-tight junction. The researchers are planning future efforts to identify which specific surgical maneuvers lead to increased stricture risk, so they can be avoided or mitigated.
“At Cleveland Clinic, we’re already adapting ICUD techniques where the robotic instruments only touch a portion of the ureter that is going to be subsequently excised, to avoid compromising vascularity,” Dr. Ericson says.
Considering the correlation between surgical experience and UEAS incidence, the study’s authors conclude that sufficient training is crucial.
“Many community-based urologists already are opting to refer patients needing cystectomy to high-volume centers,” Dr. Ericson says. “Our message isn’t that ICUD should only be performed at these centers, but that if you’d like to adopt the ICUD approach, fellowship training or mentorship from an ICUD-experienced surgeon is appropriate.”
Advertisement
Advertisement
Meet Dr. Andreas Alexopoulos
Study offers evidence to guide treatment decisions
Assessments of the shorter collection routine are encouraging, but not yet definitive