Cleveland Clinic program to streamline clinical care and research

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b8286235-5835-4d52-982a-fa955d7f7f72/22-DDI-3242262-Neuroendocrine-Tumor-Kim-3-hero_jpg)
22-DDI-3242262 – Neuroendocrine Tumor-Kim-3-hero
“No one sets out to specialize in something as rare as neuroendocrine tumors,” says Michelle Kang Kim, MD, PhD, Chair of Cleveland Clinic’s Department of Gastroenterology, Hepatology and Nutrition. “Specializing in the field is usually due to a remarkable combination of environment and mentorship, and that certainly was true for me.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Dr. Kim, who currently serves as Chair of the Carcinoid and Neuroendocrine Tumor Section of the American Gastroenterological Association, was mentored by a legend in the field during her 17 years at New York’s Mount Sinai Hospital. Richard R.P. Warner, MD, Founder of the Center for Carcinoid and Neuroendocrine Tumors at Mount Sinai, had a unique clinical practice composed solely of patients with neuroendocrine tumors.
“A decade or two ago, knowledge about the diagnosis wasn’t widespread," says Dr. Kim. "Treatment wasn’t well understood, unless a patient was fortunate enough to have a physician who had seen the condition more than once in their career. Patients with neuroendocrine tumors were desperate for answers, and I saw how gratified they were when they met with Dr. Warner.”
Dr. Kim became a protégé of Dr. Warner and then a junior partner in his practice, which she inherited when he retired. Since 2010, she has devoted her career to the treatment and study of neuroendocrine tumors and has become a renowned expert, having published pioneering research on disease biomarkers like microRNA and on racial differences in treatment outcomes.
She brought her expertise to Cleveland Clinic when she joined the staff in 2022. As one of the only U.S. gastroenterologists specializing in neuroendocrine tumors, Dr. Kim has plans to further develop the clinical and research program at Cleveland Clinic.
Because the incidence of gastroenteropancreatic neuroendocrine tumors has been increasing (possibly due to an increase in endoscopies and scans or other factors not yet identified), it’s important for gastroenterologists to be able to diagnose the rare disease and know what to do, says Dr. Kim.
Advertisement
“Chances are good that gastroenterologists today will see these tumors at some point in their career,” she says.
Education about these rare malignant tumors has progressed in the past 10-15 years, says Dr. Kim, although she still occasionally hears medical professionals refer to the tumors as benign.
“All neuroendocrine tumors are cancer, although at the time of presentation some tumors may not yet be invasive or otherwise demonstrate malignant behavior,” she says. “Some neuroendocrine tumors can cause substantial morbidity and mortality.”
“Carcinoid tumors,” while sometimes used as a synonym for “neuroendocrine tumors,” are actually a subset of neuroendocrine tumors. They typically emerge in the small intestine. Carcinoid tumors cause clinical carcinoid syndrome — symptoms that can include hot flashes — associated with overproduction of certain hormones. Less than 10% of neuroendocrine tumors are carcinoid.
“Years ago, it was commonly believed that there weren’t great treatments for neuroendocrine tumors,” says Dr. Kim. “Actually, there are wonderful treatments. That’s why it’s important for patients to be seen in a high-volume center, where we know exactly how to treat the condition. It can mean a world of difference in what is recommended to patients and, ultimately, their outcomes.”
Neuroendocrine tumors can arise throughout the body, including in the lung and pancreas, but most commonly in the gastrointestinal (GI) tract (specifically the large intestine, small intestine and appendix).
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a8f5b632-93a1-4e95-876e-9c4c23f6a958/22-DDI-3242262-Neuroendocrine-Tumor-Kim-1-inset_jpg)
Pathologic specimen of a multifocal small bowel carcinoid tumor in a segment of surgically resected small bowel.
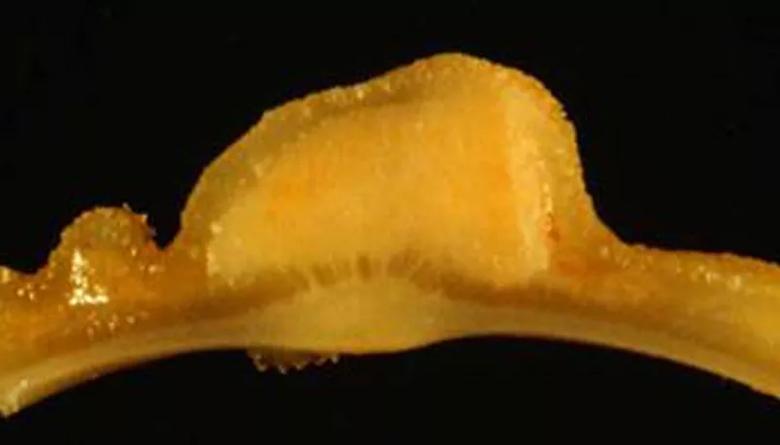
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a5f5f636-4a4b-46c8-8334-7ad7434025ab/22-DDI-3242262-Neuroendocrine-Tumor-Kim-2-inset_jpg)
Cross section of a small bowel carcinoid tumor.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/856e4f2c-beb9-405c-b199-4a3339982d55/22-DDI-3242262-Neuroendocrine-Tumor-Kim-3-inset_jpg)
Upper endoscopy with gastric neuroendocrine tumor.
While it’s rare for a gastroenterologist to specialize in neuroendocrine tumors, it’s helpful because many patients with the tumors have GI symptoms. Most neuroendocrine tumor experts in the U.S. are surgeons, oncologists or other medical specialists, notes Dr. Kim, whose practice focuses on gastroenteropancreatic tumors but also includes patients with some non-GI tumors.
“Gastroenteropancreatic tumors can mimic irritable bowel syndrome and other GI conditions,” she says. “Often I’ll counsel GI physicians — who are usually the first to see these patients — and encourage them to consider neuroendocrine tumor as a differential diagnosis if the patient doesn’t appear to be responding to an initial course of treatment. Diagnosing a tumor isn’t difficult. The difficult part is remembering to consider a tumor among other diagnostic possibilities.”
Neuroendocrine tumors are typically low grade, “cancers in slow motion,” says Dr. Kim. They may not require chemotherapy, but rather endoscopy or surgery — procedures that gastroenterologists are primed to perform.
“Oncologists are best suited to manage high-grade, more aggressive tumors,” she adds.
Since Dr. Kim began studying these tumors 17 years ago, there has been a profound transformation in their diagnosis and treatment. Research used to be mostly retrospective, single-center studies, she says. Now, large randomized controlled studies have become more common, spurred by international collaboration on care trends.
Advertisement
The power of collaboration also is evident at Cleveland Clinic, where there are a number of physicians with an interest in neuroendocrine tumors.
“Currently, the expertise is scattered across disciplines, which is common for multidisciplinary diseases like cancer,” says Dr. Kim. “I have met with a number of Cleveland Clinic providers who are enthusiastic about working together clinically and combining their expertise in this rare disease. I hope to help facilitate these collaborations in a growing Neuroendocrine Tumor Clinical Care and Research Program.”
While neuroendocrine tumor boards already exist at Cleveland Clinic, they occur in endocrinology, hepatology, general surgery, and other departments and institutes. Dr. Kim hopes to merge these meetings into a unified program, where all disciplines intersect.
“We already have a perfect assembly of specialists here and a large volume of patients with neuroendocrine tumors, so it will be a natural evolution,” she says. “Within two months of joining Cleveland Clinic, I already had a full clinic of patients.”
The new program will include survivorship care for patients with indolent disease. On average, an estimated 77% of people with neuroendocrine tumors are alive five years after diagnosis.
“There can be a lot of uncertainty when a patient is diagnosed with a neuroendocrine tumor,” says Dr. Kim. “They typically wonder: Will I need surgery or chemo or another therapy? What will my life look like now? How do I live with this tumor? As a provider, telling patients that I will be with them from diagnosis through all treatments and beyond is reassuring to them.”
Advertisement
In addition to ensuring quality patient care, the program will further education and research. Training and mentoring Cleveland Clinic faculty, staff, residents and fellows are important to Dr. Kim, who strives to increase awareness of the disease.
“Neuroendocrine tumors offer a fantastic opportunity for junior faculty who are interested in GI cancers and looking for an area in which to specialize,” she says.
Opportunities also exist in advancing science in the specialty, whether finding new biomarkers, personalizing care or doing predictive modeling. Dr. Kim’s first step is to grow the neuroendocrine tumor registry and biobank at Cleveland Clinic. These resources will fuel translational research, driving better understanding of the disease and its response to certain therapies. Artificial intelligence may help researchers analyze the burgeoning data to guide development of new diagnostic and therapeutic tools.
“I envision that this program will serve as a hub for patients and healthcare teams managing neuroendocrine tumors,” says Dr. Kim. “I think we can have a high-quality, high-volume program unlike any other in the U.S. I’m very excited for the future here.”
Learn more in our recent podcast.
Advertisement
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality