Guidance for treatment, including the role of post-ICU recovery clinics

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3249a892-3b40-41dd-b692-5aac90774e45/PSX_5757908_03-05-25_163_MLC)
22-NEU-2768409_neuropsych-treatment_650x450
By Erin A. Dean, MD; Michelle Biehl, MD; Kathryn Bash, APRN, CNP; Jeremy Weleff, DO; and Leopoldo Pozuelo, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This is part two of a two-part article reprinted (without references) from the Cleveland Clinic Journal of Medicine (2021;88[12]:669-679). The open-access and fully referenced original article is available at ccjm.org/content/88/12/669.
Millions of patients are admitted to the intensive care unit (ICU) annually in the United States. Considering the increased rates of ICU survival (currently 71% to 90%) and the growing elderly population, more people are likely to use ICU resources. Any survivor of an ICU stay is susceptible to health problems that continue to persist after discharge and may lead to post-intensive care syndrome (PICS). As outlined in part one of this two-part article, PICS is defined as new or worsening dysfunction in one or more of the following domains:
This review focuses on neuropsychiatric aspects of the care of ICU survivors. Part one explored neuropsychiatric diagnostic and screening recommendations; this part covers treatment recommendations and the value of post-ICU recovery clinics.
There are several intervention strategies for management of cognitive and emotional disturbances. While some treatments are for specific post-ICU impairments, many are useful in managing symptoms spanning multiple domains of PICS. Many critical care units have adopted the ICU Liberation Bundle (A-F) to prevent delirium, prolonged cognitive impairment and significant post-ICU psychiatric symptoms. The bundle consists of the following:
Advertisement
Prolonged post-ICU cognitive impairment may warrant further investigation. Physical, cognitive and vocational rehabilitation have been studied in patients with ongoing cognitive dysfunction. In the Returning to Everyday Tasks Utilizing Rehabilitation Networks (RETURN) study, cognitive rehabilitation was delivered in the patient’s home once every two weeks over a 12-week study period. ICU survivors suffering from post-ICU cognitive impairment who received post-discharge cognitive rehabilitation in addition to “usual” post-discharge care (physical rehabilitation, occupational rehabilitation, nursing care) showed improvement in cognitive function at three-month follow-up compared with patients who did not undergo cognitive rehabilitation.
Given variability of cognitive interventions and studied populations, evidence-based recommendations for clinical practice are difficult to determine. There are promising data for the role of aerobic exercise in improving post-ICU cognitive function, and neurocognitive testing has been employed for patients with prolonged cognitive impairment. However, barriers to assessing cognitive function — and thereby providing care to this population — include social stigmatization and financial strain, loss of patients to follow-up and patient frustration over testing performance. Of note, there are limited data on the role of these strategies in preventing prolonged cognitive impairment in critical care patients.
Few studies have investigated pharmacologic treatments for cognitive impairment in ICU survivors specifically. Current strategies are from studies of cognitive impairment treatment in patients with traumatic brain injury. Methylphenidate and donepezil have been studied in the traumatic brain injury population and were associated with improvement in memory and attention. Although these strategies may be considered for ICU survivors with cognitive impairment, they should be implemented cautiously as further investigation is warranted for the critical care population specifically. Rosuvastatin was studied in the prevention of delirium and cognitive impairment in ICU patients but was not found to have significant benefit in prevention.
Advertisement
Psychotherapy may be beneficial for psychiatric symptom management in ICU survivors. The patient’s presenting psychiatric symptoms may guide the type of therapy recommended. For example, some patients with mild symptoms of depression, anxiety or post-traumatic stress disorder (PTSD) may benefit from supportive therapy. Moderate to severe mood and anxiety symptoms may respond more appropriately to cognitive behavioral therapy, while patients with more advanced trauma symptoms may benefit from trauma-based therapy, including but not limited to eye-movement desensitization and reprocessing, a form of psychotherapy that allows patients to access and process traumatic memories through simultaneous focus on external stimuli such as eye movement.
Haerizadeh et al. reviewed psychological treatment modalities for PTSD in medically ill patients. Although limited data were available, two of the included trials showed exposure-based cognitive behavioral therapy resulted in a lower incidence of PTSD symptoms compared with control groups. And three of the included trials found eye-movement desensitization and reprocessing to be more effective in reducing PTSD symptoms than relaxation therapy, imaginal exposure and conventional cognitive behavioral therapy.
Patients with more severe psychiatric symptoms may warrant pharmacologic management. There is a lack of literature analyzing pharmacologic treatment for depression, anxiety and PTSD in ICU survivors. It is important to note that ICU survivors warrant ongoing monitoring by a primary care provider or mental health clinician as they may be more sensitive to medication side effects given their underlying medical comorbidities and potential risk of drug interactions with other medications.
Advertisement
ICU diaries are used to fill memory gaps for ICU survivors and provide an understanding of ICU events in a chronologic or narrative account. The diaries are often completed by ICU staff, including physicians, advanced practice providers, nurses, consultants and others involved in ICU patient care (e.g., physical therapists, occupational therapists, music therapists, art therapists). Families may also participate in construction and completion of the ICU diaries.
ICU diaries have been increasingly used as a management strategy for emotional disturbances of PICS in ICU survivors. Data analyzing effects of ICU diaries on psychiatric symptoms in ICU survivors have been mixed. Barreto and colleagues found that the use of ICU diaries was associated with decreased rates of depressive symptoms and depression diagnoses, mostly beneficial in ameliorating anxiety symptoms, but did not significantly improve PTSD symptoms. Garrouste-Orgeas et al. found no statistically significant benefit in reduction of PTSD symptoms from use of ICU diaries in mechanically ventilated ICU patients at three-month follow-up.
Of note, there is no universal template for ICU diaries. They are unstructured documents to be used by the patient and, after discharge, also by the family if the patient so chooses.
PICS symptoms after an ICU stay have led to a reevaluation of methods of care. Traditionally, within one month of hospital discharge, ICU survivors would have a brief follow-up visit with their primary care provider to address the complexities of a potentially extended critical care hospitalization. However, the time constraints of a brief office visit increased the risk that the patient’s complex post-discharge needs would be suboptimally addressed.
Advertisement
Recognizing these issues, critical care providers have developed post-ICU recovery clinics in which ICU survivors can receive outpatient follow-up care targeted to their needs. These clinics are composed of multidisciplinary teams usually including, but not limited to, critical care specialists, physical therapists, case managers, social workers, respiratory therapists, pharmacists and mental healthcare professionals such as psychiatrists and psychologists.
Reported outcomes of post-ICU clinics have been positive overall in improving depression, anxiety, and PTSD symptoms. Also, qualitative outcomes have revealed positive results for patients and families, who reported higher levels of satisfaction from involvement in these clinics.
The Post-ICU Recovery Clinic (PIRC) at Cleveland Clinic (Figure) involves an ICU physician, ICU advanced practice provider, pharmacist, physical therapist and respiratory therapist, along with mental health providers. Patients are triaged as they are discharged from the ICU based on the following criteria:
Patients who meet inclusion criteria are tracked while on the regular nursing floor to capture discharge disposition; patients discharged to skilled nursing facilities are not eligible for the clinic. The PIRC project manager consults with the patient to discuss PICS and the PIRC. If the patient expresses interest, a post-discharge PIRC visit is scheduled. The goal is to see patients in the clinic within four weeks after hospital discharge.
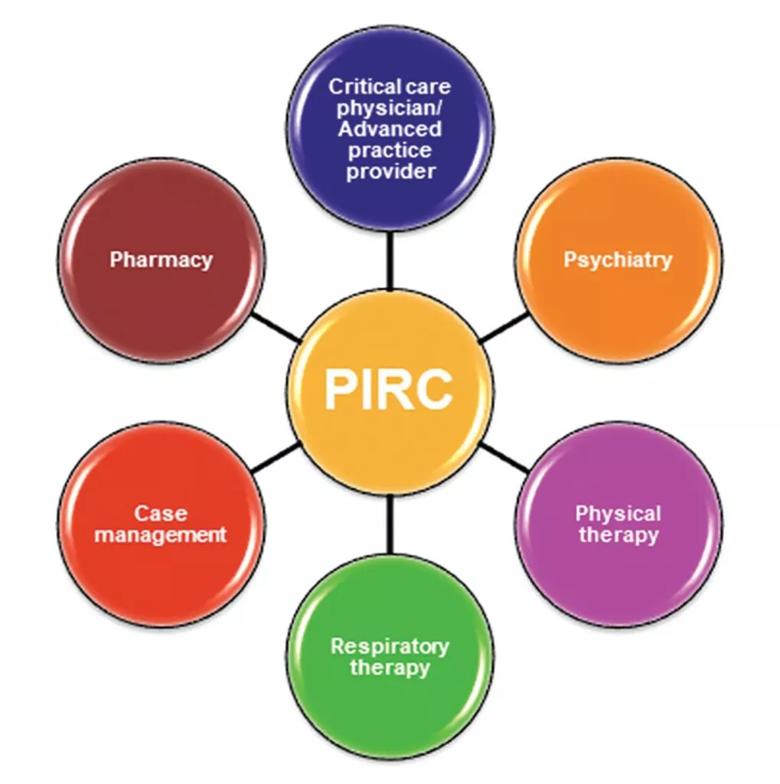
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8576ef46-2f8d-4dbc-986a-18ff50ce9744/22-NEU-2768409_inset-1019x1024_jpg)
Figure. The multidisciplinary team approach used in the Cleveland Clinic Post-ICU Recovery Clinic (PIRC).
During the post-discharge PIRC visit, several screening tools (see part one of this article) are used to determine the patient’s level of physical, cognitive and emotional impairment. Based on the patient’s symptom severity as determined by screening tools and personal interviews, a referral may be made to a clinical psychologist for psychotherapy or to a consultation psychiatrist for medication management. If patients show cognitive impairment based on screening or are reporting significant cognitive dysfunction compared with their pre-ICU baseline, a referral is made to neuropsychiatry for further symptom management.
Neuropsychiatric symptoms are prevalent and at times disabling in ICU survivors. Previously, survivors have been at increased risk of psychiatric symptoms going undetected owing to limitations in post-discharge follow-up, mental health stigma, and limitations in financial and social circumstances due in part to acute and chronic medical conditions. ICU survivor neuropsychiatry is an emerging field that continues to be evaluated and is even more pressing in the COVID-19 era.
Clinicians seeing patients in the ICU and in the outpatient setting should be knowledgeable about the potential for PICS and appropriate screening tools for patient monitoring. Even with the advances made in identifying screening tools in ICU respiratory survivors, further studies are warranted to evaluate these and other assessments for neuropsychiatric symptoms of PICS across various diagnoses and conditions in ICU survivors.
Another area of continuing research is that of the post-ICU clinic in investigation of long-term outcomes of PICS, including long-term prevalence of neuropsychiatric symptoms, treatment strategies, mortality rates, readmission rates, financial impact for the healthcare system, and patient and caregiver satisfaction. These clinics allow for collaborative care not only in the areas covered in the Cleveland Clinic PIRC but also with geriatric medicine, otorhinolaryngology, endocrinology, nutrition, psychology, neuropsychiatry and neuropsychology. Establishment of post-ICU clinics allows clinicians and researchers to further investigate treatment modalities and prevention strategies and to improve care for ICU survivors.
This is part two of a two-part article reprinted from the Cleveland Clinic Journal of Medicine (2021;88[12]:669-679). The open-access and fully referenced original article is available at ccjm.org/content/88/12/669.
Dr. Dean is a staff physician, Dr. Weleff is a PGY4 resident, and Dr. Pozuelo is Department Chair, all in Cleveland Clinic’s Department of Psychiatry and Psychology. Dr. Biehl is Director of the Post-ICU Recovery Clinic and Ms. Bash is a certified nurse practitioner, both in Cleveland Clinic’s Department of Pulmonary and Critical Care Medicine.
Advertisement
New study highlights the need for plain-language prompting and human oversight in addiction care communication
What hospital clinicians get right — and wrong — when diagnosing depression and delirium
Swift, aggressive thiamin therapy may be key to preventing long-term neurological injury
Case underscores potential dangers of combining psychedelics with tranylcypromine and stimulant medications
Researchers explore how changes in the gut microbiome influence the brain's reward response to alcohol
Researchers explore new avenues for the management of psychiatric illness in patients with seizure disorders
Addiction experts use decades of research and clinical experience to help patients overcome substance use disorders
Specialized course helps APPs navigate clinical concerns and interpersonal skills