System based on clinical symptoms and their duration

From nausea and vomiting to frank abdominal distension, patients undergoing elective colorectal surgery can experience a wide spectrum of postoperative gastrointestinal dysfunction. There are also varied approaches to prevent or treat these outcomes in clinical practice with little published in the literature to standardize the definition or effective therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That is, until now. Cleveland Clinic colorectal surgeon Stefan Holubar, MD, and colleagues created a consensus statement that aims to remove the ambiguity around postoperative gastrointestinal dysfunction (POGD) ― traditionally known as ileus ― in both clinical and research settings.
“This is really a bit of a breakthrough in the field of abdominal surgery, not just colorectal surgery. There is a very loose definition of ileus; it varies from study to study,” Dr. Holubar says. “The consensus statement provides a nascent, new de facto definition for the spectrum of GI dysfunction.”
The consensus statement authors propose the i-FEED scoring system based on clinical symptoms and their duration; including nausea or vomiting; physical examination findings; abdominal distention with tympany; and more. In a very practical sense, the score calculation corresponds to a stoplight color-coded system:
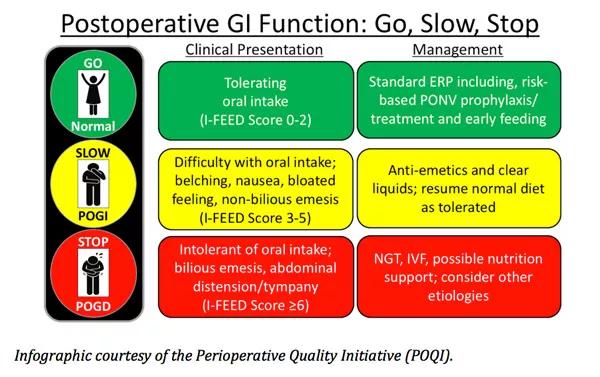
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6fa839ab-4368-467f-8fb7-f70da252d382/18-DDI-098-Concensus-Statement-CQD-inset_jpg)
This i-FEED scoring system and GO-SLOW-STOP management strategy could help guide treatment for the 10 to 20 percent of colorectal surgery patients who experience some form of postoperative dysfunction.
When a patient scores very low, less than 3, they can have early feeding after surgery, receive prophylaxis for postoperative nausea/vomiting prophylaxis and can continue to eat. That’s the green or ‘go’ on the stoplight. For those who score in the middle, 3 to 5 points on i-FEED, it’s suggested that they slow down. That’s the yellow category where patients report some symptoms of GI intolerance, Dr. Holubar explains. “And we do recommend that the patient take multiple anti-emetics and back down to a clear liquid diet.”
Advertisement
However, an i-FEED score of greater than or equal to 6, which indicates frank GI dysfunction, means the patient is not able to tolerate oral intake or has abdominal distention with tympany. In terms of management, insertion of a nasogastric tube and/or intravenous fluids may be warranted. In addition, it’s important for clinicians to rule out other etiologies of postoperative GI dysfunction, Dr. Holubar says.
The joint consensus statement comes from the American Society for Enhanced Recovery and the Perioperative Quality Initiative, and addresses how enhanced recovery pathways can improve patient experience and surgical outcomes.
“The enhanced recovery pathways actually begin before surgery, when you meet the patient and set expectations for a shorter length of stay, reduced pain with opiate sparing or opioid free anesthesia and analgesia,” Dr. Holubar says. Additional features include use of around-the-clock acetaminophen, anti-inflammatories and long-acting local anesthetics, and multimodal pain management to avoid prescription of opioids.
“Despite all this, people still get what is formally known as ileus … [although] we try to use postoperative GI dysfunction as a more modern term,” Dr. Holubar says.
The enhanced recovery principles and the POQI consensus statements are geared to all different types of institutions, from community hospitals to major referral centers like Cleveland Clinic. By adopting enhanced recovery pathways, “we have moved the needle here at Cleveland Clinic for elective and non-elective colorectal procedures” in terms of quality, safety, outcomes and cost, Dr. Holubar says.
Advertisement
“Similar to laparoscopic surgery, we often have to spend a little more to do enhanced recovery, but the shorter length of stay pays for itself, and pays off as an excellent return on investment.”
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications