Three presentations from the DDW 2023 conference help identify best candidates and illustrate the positive impact redo IPAAs can have on a patient’s QoL
Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA), the preferred procedure among patients with ulcerative colitis, is associated with a variety of early and late complications that can lead to pouch failure in 5% to 15% of cases. Individuals faced with pouch failure, and who are motivated to maintain intestinal continuity, may choose to undergo a redo IPAA procedure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Ultimately, the choice to undergo a permanent ileostomy versus a redo IPAA is a quality of life decision,” says Tracy Hull, MD, Staff Surgeon in the Department of Colon and Rectal Surgery at Cleveland Clinic, while noting that the research regarding the long-term impact and functional outcomes post-redo IPAA remain limited. “Since this decision is often based on patient preference, focusing on quality of life and patient-reported outcomes is critical.”
With this is mind, lead study author Marianna Maspero, MD, Research Fellow at Cleveland Clinic, Dr. Hull, the corresponding author, and colleagues conducted several studies exploring key areas related to redo IPAAs, including quality of life. Findings from these research efforts were recently presented during the Digestive Disease Week conference.
The Cleveland Clinic is one of the highest-performing institutions when it comes to primary and redo IPAAs, according to Dr. Maspero. “Patients undergoing index or redo IPAAs are given the Cleveland Clinic Quality of Life Instrument (CGQLI) at each follow-up visit,” she explains. “As a result, we have a large pouch registry with quality of life data.”
Using data from this prospectively collected redo pouch registry, Dr. Maspero and the Cleveland Clinic team examined the quality of life among patients who underwent redo ileoanal pouch surgery.1 Patients included in the analysis had completed at least one CGQLI following their procedure.
Among 374 eligible patients, 879 CGQLI were available. Fifty-seven percent were female and the median age at redo pouch was 40 years. Study investigators noted a median interval between redo pouch and the latest CGQLI of five years.
Advertisement
Data showed an overall CGQLI score (0-1) of 0.7 (0.5-0.8). Dietary, social, work and sexual restrictions were reported in 50%, 34%, 38% and 37% of patients, respectively. The median happiness score with surgery among patients was eight out of ten.
At the latest follow-up, 56 (15%) patients had an ileostomy, according to Dr. Maspero, who noted that sexual restrictions were higher with ileostomy while happiness with surgery was lower, but all other quality-of-life domains were similar. When looking at trends, the researchers found that quality of life was lowest during the first postoperative year and then significantly increased at three, five, and 10 years after redo surgery.
Given these findings, the study authors concluded the majority of patients with a redo pouch maintained intestinal continuity with sustained quality of life. “Understanding the impact redo IPAAs have on the quality of life is important for patient counseling and decision making,” says Dr. Maspero. “And the fact that the quality of life and functional outcomes, for the most part, stayed the same over time is a reassuring message for patients considering this option.”
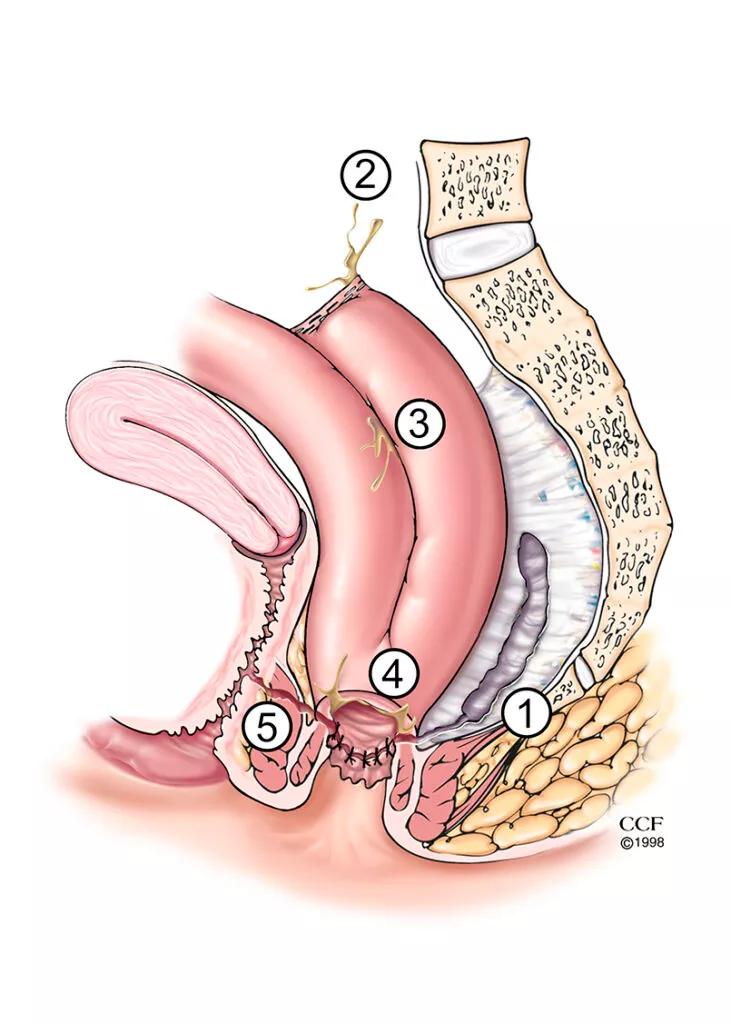
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/92e51603-7837-45d1-b747-550dd13957e5/23-DDI-3722063-CQD-Inset1-731x1024_jpg)
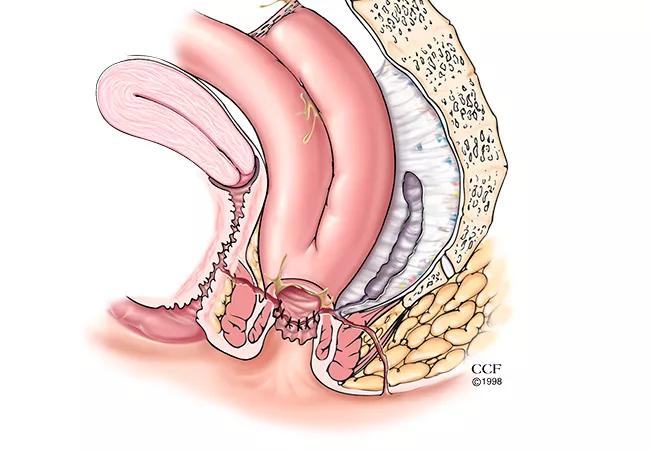
Illustration of common IPAA complications. Left panel, 1 = presacral sinus, 2 = leak from tip of the J-pouch, 3 = leak from body of the J-pouch, 4 = pouch-anal anastomotic leak with transphincteric fistula-in-ano, 5 = pouch-vaginal fistula.
After a redo IPAA, pouch failure occurs in 20% to 40% of cases. The decision to proceed with a second redo procedure is currently a controversial one. Given the limited evidence regarding the long-term pouch survival and functional outcomes of this approach, Dr. Maspero and colleagues examined Cleveland Clinic’s experience with second redo IPAA procedures.2
Advertisement
The researchers retrospectively analyzed data from their pouch registry. All patients who underwent a second redo IPAA procedure from 2004 to 2021 were identified. The primary outcomes of this study was pouch survival—defined as no pouch excision or rediversion — as well as patient-reported outcomes measured using the Cleveland Global Quality of Life survey.
Twenty-three patients were included in this analysis. The majority of patients had an index diagnosis of ulcerative colitis (87%) and the remaining had indeterminate colitis (13%). The final diagnosis of eight patients (35%) was changed to Crohn’s disease.
The researchers reported that the indication for pouch salvage was the same for the first and second redo in 21 (91%) cases. Twenty patients underwent both redo IPAAs for septic complications. After a median follow up of 39 months, seven (30%) patients experienced pouch failure, according to Dr. Maspero and colleagues, who observed an overall pouch survival at three years of 76%.
In terms of quality of life, the data showed that urgency occurring most days of the week was reported by 14% of patients, any incontinence by 29%, and any seepage was reported in the daytime by 71% and at night by 86%.
When compared with a group of redo IPAA patients, similar quality of life and functional outcomes were observed, suggesting that a second redo pouch procedure is a viable option with acceptable outcomes for select patients who are highly motivated to maintain intestinal continuity, says Dr. Maspero.
Advertisement
The cause of pouch failures following restorative proctocolectomy with IPAA can have an impact on the success rate of the redo pouch, and septic complications are linked to a higher risk of failure than other etiologies.
However, more study is needed to understand if the timing of pouch failure (early versus late) has an impact on long-term outcomes for redo IPAA following sepsis-related complications. Dr. Maspero and colleagues performed a retrospective analysis of their institutional pouch database with a primary endpoint of pouch survival.3
Patients who received a redo IPAA for septic complications between 1988 and 2020 were divided into two groups: early (n=241) and late failure (n=94). The researchers defined early failure as pouch failure within six months of stoma closure after index operation, or stoma never closed. Pouch failure after six months of stoma closure was considered a late failure.
Data revealed that the most common indication for failure was anastomotic leak in the early failure group (68%) and fistula in the late failure group (63%). The study authors reported that pouch survival at three-, five-, and 10-years was 77%, 75% and 72% among patients with early failure, and 79%, 75% and 68% for the late failure group, respectively. Additionally, findings demonstrated that fistula was the most common reason for redo pouch failure in both groups. Patients with early and late failure had similar quality of life.
These findings demonstrated comparable outcomes after a redo IPAA between patients with early and late sepsis-related index pouch failure. This was a surprising outcome, according to Dr. Maspero and colleagues, who hypothesized that late pouch failure would be associated with worsened outcomes.
Advertisement
“This is an interesting — and reassuring — finding for individuals who may be candidates for a second redo IPAA,” notes Dr. Maspero, who emphasized that this approach is not going to be the right choice for everyone but select patients could benefit.
These studies underscore the importance of continued data collection as well as patient-reported outcomes. “The work Cleveland Clinic is doing with quality of life data is very important, and something that should be implemented across the board,” says Dr. Maspero.
“Access to a large body of quality of life data adds value not just to our research, but also for our patients,” she concludes. “Tools like the Cleveland Clinic Quality of Life Instrument help patients feel heard and provide clinicians with additional information to ensure comprehensive care.”
References
Advertisement

Retrospective analysis looks at data from more than 5000 patients across 40 years

A proof-of-concept study shows how 3D pouchography can be a useful adjunct for surgeons

Radiation to the pelvis from cancer treatment made the traditional treatment path unavailable
A new study illustrates why it’s important for clinicians to be aware and suspicious of tip of the J-pouch leaks

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling