Study sheds light on distant metastasis rates between upfront surgery and Watch & Wait strategies

New findings show that patients who experience local regrowth after total neoadjuvant therapy (TNT) and a Watch & Wait (WW) management approach are not at a higher risk for distant metastasis than those who have upfront surgery after TNT. The findings were presented at this year’s American Society of Colon and Rectal Surgeons Annual Scientific Meeting in San Diego.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
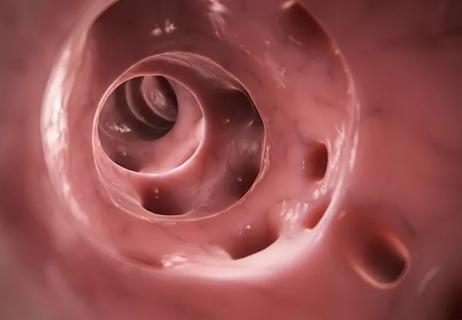
“Over the last decade, there’s been a paradigm shift in colorectal cancer management towards prioritizing organ preservation,” explains Emre Gorgun, MD, MBA, Vice Chair, Colorectal Surgery at Cleveland Clinic and senior author on the paper. “Findings from two earlier studies, the PRODIGE 23 and RAPIDO trials, demonstrated how TNT was beneficial to patients in the long term, and then the OPRA trial showed how TNT could lead to better organ preservation.”
He continues, “The findings from these three studies really led to providers taking a WW approach to colorectal cancer management, but there were concerns about how delaying surgery with WW could lead to a higher metastatic risk of distant regrowth. Our study was essentially looking at whether local regrowth after achieving a complete clinical response in patients treated with TNT increases the risk of distant metastasis. Additionally, we also wanted to evaluate whether this risk could be reduced by upfront surgery performed after TNT.”
The single-center retrospective cohort study included 74 patients with locally advanced rectal cancer who received TNT between 2018 and 2024. Of these, 32 achieved an initial complete clinical response (cCR) after TNT, were managed with a WW approach, but subsequently developed local regrowth with required a salvage total mesorectal excision (TME). The remaining 42 patients underwent upfront TME following an incomplete clinical response but were found to have a pathologic near-complete response.
Advertisement
After a median follow-up of 29.3 months in the upfront surgery group and 23.3 months in the local regrowth group, seven patients in each group developed distant metastases (P = .57). Statistical analysis showed that there was no significant difference between the two groups as far as distant metastasis–free survival rates from the end of TNT. However, perineural invasion and incomplete mesorectal excision were significantly associated with increased risk of distant metastasis, and ypT3–4 stage was a significant predictor of distant metastasis. On the other hand, complete mesorectal excision was independently protective.
“Our findings demonstrated that TNT and a WW approach with these patients is safe,” says Dr. Gorgun. “Even in local regrowth cases that were followed by salvage surgery, the risk of distant metastasis was not significantly different compared to patients who underwent upfront TME. But the quality of the surgery is a major factor, and we found that an incomplete mesorectal excision was associated with increased risk of distant metastasis.”
He continues, “The finding that incomplete mesorectum might be a marker and a modulator of disease aggressiveness really highlights the value of high-quality surgical technique. Given this, patients with local regrowth might benefit from referral to centers with significant expertise in complex pelvic dissection. At Cleveland Clinic, our surgical team performs hundreds of these surgeries a year, and our multidisciplinary approach to care relies on the input from several specialties to ensure the best outcomes for patients. Our Center for Young-Onset Colorectal Cancer also specializes in care for patients under 50, and unfortunately, we’re seeing rising incidence rates among this age group.”
Advertisement
Dr. Gorgun believes that while these findings won’t necessarily change how care is provided at Cleveland Clinic, they do provide confirmation that what his team has already been doing is beneficial. However, he suggests that these findings may prompt longer observational periods for patients to ensure there is no regrowth. Eventually, he hopes that more steps can be taken to better identify patients at risk of regrowth. He believes biomarkers could potentially identify patients who respond well to treatment and those who might be at higher risk of regrowth or distant metastasis.
The study, “Risk of Distant Metastasis in Rectal Cancer: Local Regrowth vs. Upfront Surgery after TNT with Near Complete Response,” was presented at the 2025 American Society of Colon and Rectal Surgeons (ASCRS) Annual Meeting.
Advertisement
Advertisement

Poor response may be due to different tumor biology

Tips on how to recognize the condition and budesonide treatment guidance

Findings could help promote organ preservation
Input from specialists and other healthcare providers is important when discussing quality-of-life improvement options

The retrospective study also identified predictors for which patients would likely achieve a complete response from TNT

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence