A rare form of sarcoma treated by cytoreductive surgery
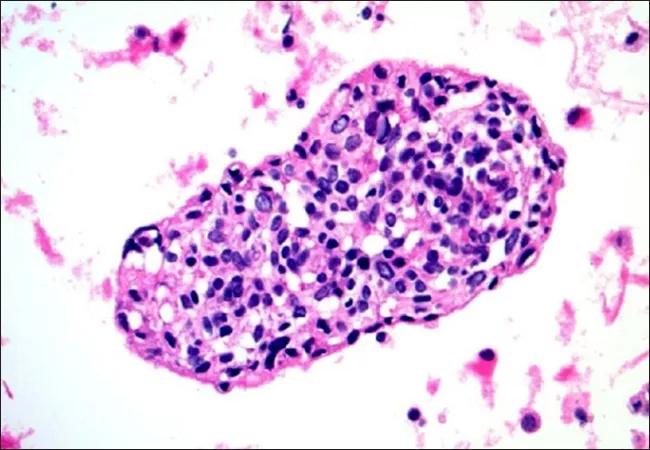
Desmoplastic small round cell tumor (DSRCT) is a rare and aggressive form of sarcoma with the greatest incidence in children, adolescents and young adults. In this Consult QD article, Cleveland Clinic Children’s pediatric oncologist Peter Anderson, MD, PhD, discusses the recent advances in treating this rare tumor and his own clinical experience with patients with DSRCT.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This is a very difficult solid tumor to treat. It belongs to the Ewing’s family of tumors, but unlike the standard Ewing’s tumor, the Wilms’ Tumor-1 (WT-1) and Ewing sarcoma (EWS) genes are fused, which gives DSRCT some Ewing’s characteristics as well as some unique and difficult-to-treat characteristics,” he says.
According to Dr. Anderson, the unique features of DSRCT include a disproportional incidence in young men and the presence of large numbers of intraabdominal metastases.
“About 90 percent of the patients are men, so some sort of interaction of neuroendocrine nature is probably at play. Furthermore, the patients often present with a very large number of abdominal metastases — sometimes in the hundreds,” he says, adding “the major challenge is getting patients to as low of a disease burden as possible using chemotherapy, at which point surgery can significantly contribute to the cure.”
In an article published recently in the Annals of Surgical Oncology, Dr. Anderson and his colleagues from MD Anderson Cancer Center led by Andrea A. Hayes-Jordan, MD, reported the results of a phase 2 clinical trial that examined the effectiveness of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS-HIPEC) with cisplatin in 20 patients with sarcoma (14 with DSRCT and five with other sarcomas; one patient with DSRCT had repeat CRS-HIPEC and enrolled twice). All patients received the recommended phase 2 dose of cisplatin (100 mg/m2) for 90 minutes at 41°C as part of closed-technique HIPEC.
Advertisement
“My role in this study was to get the patients in good enough shape so that surgery was possible, and to work with Dr. Hayes-Jordan and other surgeons to make sure that patients after surgery continue to get therapy at the basis,” Dr. Anderson says.
“In our study, patients with DSRCT had significantly longer median overall survival (OS) after cytoreductive surgery compared with patients with other sarcomas, (44.3 vs. 12.5 months, P = 0.0013),” Dr. Anderson notes, adding that recurrence-free survival (RFS) was also significantly longer for patients with DSRCT compared with patients with other tumors (14.9 vs. 4.5 months, P = 0.0012). “Thus, aggressive surgery seems to provide a ‘gift of time’ to DSRCT patients,” he says.
Dr. Anderson says “this trial has shown that not only is cytoreductive surgery technically feasible, but we also know what dose of cis-platinum to use. Too little cis-platinum will not achieve the desired effect and too much will cause problems with kidney dysfunction.” In terms of treatment expectations, Dr. Anderson believes the study “has set a minimum for what should be expected by a DSRCT patient — to get to a low disease burden.”
At Cleveland Clinic, Dr. Anderson is currently focusing on reducing the chances for relapse in DSRCT patients.
“We recently treated six patients with a drug called ONC201, which Dr. Hayes-Jordan previously tested in her lab. Some patients responded and some ultimately progressed, but I think that this drug has promise in the adjuvant setting and the potential for use in relapse prevention,” he says. “We have one patient who has said this is the best she has felt in more than three years and she continues to respond, more than six months on the well-tolerated ONC201 drug.”
Advertisement
According to Dr. Anderson, getting a consultation from an expert who is familiar with the principles of therapy for DSRCT is one of the most important steps in treating a very rare tumor such as DSRCT. Cleveland Clinic is facilitating this process by offering HIPAA-secure virtual visits to patients who live not only in Ohio, but also other states and Canada. Dr. Anderson is very enthusiastic about the benefits of this program helping DSRCT patients know options and how to control side effects of therapy, too.
“I now perform anywhere between two and four virtual visits per week and some of those are DRSCT patients. I am very impressed with this process — how easy and friendly it is and how much information we can provide to the patients. I provide a summary, articles, clincaltrials.gov information, and often PowerPoint images, so they have a much better idea of systemic and local control options. Also, we talk about how to improve intestinal health to make chemotherapy, surgery and radiotherapy less toxic and more effective for DSRCT,” he says. “Without virtual visit access to Cleveland Clinic’s pediatric oncology and sarcoma programs, many of these patients would not have the opportunity to consult a team with extensive experience treating DRSCT.”
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient