Validation study finds survey fills an unmet need
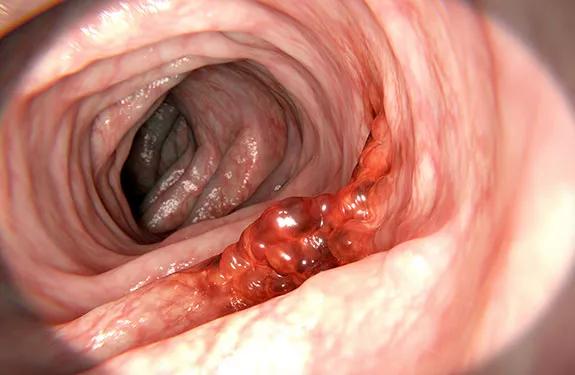
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a07008d6-cb1d-4c68-a0d3-c3af24121127/650x450-Colorectal-Cancer-GettyImages-646161486_jpg)
650×450-Colorectal-Cancer-GettyImages-646161486
A new Cleveland Clinic-developed questionnaire reliably measures quality of life in colorectal cancer surgery patients, a validation study has found. Statistician Alexandra Aiello, MSPH, presented the results at the 2019 annual scientific meeting of the American Society of Colon and Rectal Surgeons.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When compared with other available surveys, the Cleveland Clinic Colorectal Cancer Quality of Life (CCF-CaQL) questionnaire achieved validity in five key areas: construction, internal consistency, convergence, discrimination and responsiveness.
“The CCF-CaQL is a relatively concise survey covering content specific to the colorectal cancer surgery patient population,” says principal investigator and Cleveland Clinic colorectal surgeon Massarat Zutshi, MD. “We believe it will provide clinicians with a tool for predicting when complications are likely to occur, so they can counsel patients accordingly.”
A panel of experts developed the CCF-CaQL in response to the need for a comprehensive evaluation tool that took patients less time to complete than existing surveys, and that produced data more applicable to the colorectal surgery population.
The project was initiated more than a decade ago, when Cleveland Clinic was conducting a study comparing surgical procedures for colorectal cancer treatment. “We looked at all available questionnaires and found none was suitable,” says Dr. Zutshi.
Each questionnaire had strengths and weaknesses. None focused specifically on colorectal cancer surgery, and none provided a global quality-of-life score, since the areas of mental and physical health were covered separately.
To obtain a comprehensive score, patients had to fill out multiple questionnaires. Many questions did not apply to colorectal cancer or surgery, and the older tools did not take into account modern treatments that impact quality of life, such as chemoradiation and minimally invasive surgery.
Advertisement
“The surveys were either too general to be informative or too lengthy to complete,” says Dr. Zutshi
The solution was to develop a shorter but comprehensive and updated questionnaire that would enable clinicians to understand a colorectal surgery patient’s quality of life at any given point in time.
The initial CCF-CaQL contained 26 questions focusing on quality of life, pain, bowel function and patients’ concerns about the future. It was tested in a pilot study involving 20 colorectal cancer patients and 20 controls. As a result of their input, one question was removed. The remaining 25-question survey proceeded to the validation study.
In this international validation study, the researchers administered three surveys — the CCF-CaQL, the Functional Assessment of Cancer Therapy-Colorectal Cancer (FACT-C) and the Short Form Health Survey (SF-12) — preoperatively and at six, 12 and 24 months postoperatively to 190 patients with low rectal cancer who were randomized to sphincter-sparing surgery with the J-pouch procedure or side-to-end anastomosis.
When the researchers compared the results, they found that more patients completed the CCF-CaQL than the FACT-C.
With fewer questions overall than the other two surveys, yet with questions specific to the colorectal surgery population, the CCF-CaQL provided accurate, useful data specific to quality of life following colorectal cancer surgery. At 24 months post-surgery, the CCF-CaQL was able to detect a significant difference between those patients who did and did not have complications (p < 0.001), highlighting its discriminative capability.
Advertisement
“The study validated our feeling that the new survey would enable us to measure treatment options at any point in time after surgery and know how well they are working,” says Dr. Zutshi.
The survey will be made available free of charge to interested physicians.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches