Cryopreservation of oocytes and tissue plus ovarian transposition in a young woman with cervical cancer
Cleveland Clinic physicians have used three techniques in combination to help a young patient recently diagnosed with cervical cancer preserve her fertility. The case was illustrated in a video presented today at the annual meeting of the American Society for Reproductive Medicine by Cleveland Clinic’s Natalia Llarena, MD, and Mariam AlHilli, MD, together with other collaborators. The procedures performed were oocyte cryopreservation, ovarian tissue cryopreservation and ovarian transposition.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Women are born with a finite number of eggs. Chemotherapy and radiation can damage the ovaries, resulting in infertility and early menopause. Several options are available for fertility preservation; however, data show that many eligible women do not receive counseling about fertility preservation at the time of their cancer diagnosis. Options include:
“Although oocyte or embryo cryopreservation is the most reliable mode of fertility preservation, live birth rates are lower in women with cancer after this procedure,” says Dr. Llarena, who is a clinical fellow in Reproductive Endocrinology and Infertility at Cleveland Clinic. Additionally, oocyte cryopreservation does not help preserve ovarian function. “Use of the three techniques in this patient will help optimize her potential for a live birth in the future. Combining the approaches also may allow her to retain some gonadal function, which is an additional benefit.”
Advertisement
The patient, a 24-year-old G1 P0010 who was previously healthy, had been diagnosed with stage 1B1 cervical clear cell adenocarcinoma. Her planned treatment was weekly cisplatin and 45 Gy of external-beam radiation therapy delivered in 25 fractions plus brachytherapy.
In premenopausal women undergoing radiation therapy, a dose of 15Gy is estimated to result in sterilization. The woman strongly desired fertility preservation and was referred to reproductive endocrinologists at Cleveland Clinic. After thorough counseling, the patient opted to proceed with all three methods of fertility preservation.
“In this case, the patient was very young at the time of cervical cancer diagnosis and very motivated to preserve her fertility. I have also seen patients with cancer who were not offered fertility preservation for one reason or another who were regretful about that,” says Dr. Llarena. “Even if there aren’t a lot of options because of a woman’s particular cancer or treatment, counseling about fertility is important so that she understands what to expect in the future.”
The first procedure performed on this patient was ovarian cryopreservation of mature oocytes following ovarian stimulation. In women under age 38, cryopreservation of 15 to 20 oocytes is associated with a 70% to 80% likelihood of live birth. Individuals with cancer typically have time to undergo only a single cycle of ovarian stimulation. “Our patient had only nine mature oocytes retrieved, so she did not meet the benchmark for good odds of a live birth. The other options for fertility preservation allowed us to improve her chances,” says Dr. Llarena.
Advertisement
Next, the patient underwent ovarian transposition, a surgical procedure in which the ovary was placed above the anterior-superior iliac spine in a lateral location, out of the field of pelvic radiation. The surgeons dissected the woman’s ovary away from her fallopian tube and separated the ovary from the uterus. The ovary — along with its vascular blood supply — were pulled upward through a tunnel of peritoneal tissue and sutured to the abdominal wall using permanent suture and clips to allow the radiation oncologist to identify the ovary on imaging.
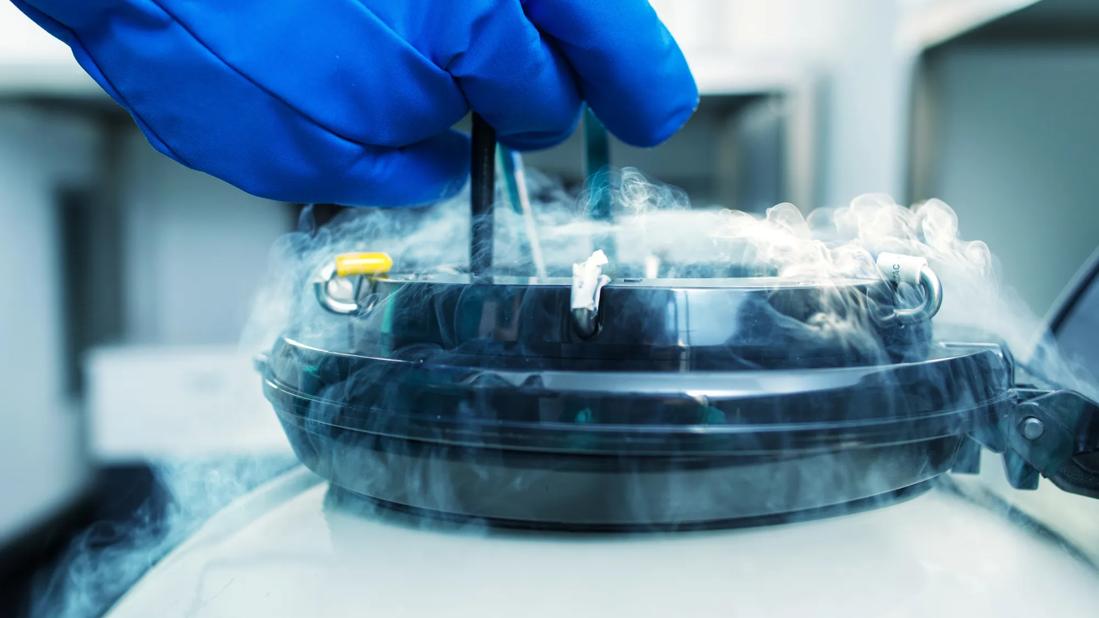
Finally, this patient underwent ovarian tissue cryopreservation at the time of the ovarian transposition procedure. The ovarian tissue was surgically removed, and transported to the lab. At that time, the ovarian tissue was cut into rectangular slices; the slices were placed in cryoprotectant and then in liquid nitrogen.
The woman’s cryopreserved ovarian tissue also can later be reimplanted into the pelvis. Pregnancy rates following such procedures in patients without ovarian metastasis range from 29% to 41%. To date, reimplantation of cryopreserved ovarian tissue has resulted in more than 130 live births and live birth rates after it range from 23% to 36%. Unfortunately, for some women reimplantation of ovarian tissue is not possible due to a risk of cancer recurrence, including those with ovarian cancer, leukemia and lymphoma. “Ovarian tissue reimplantation would not be an option for a patient with an advanced or metastatic cancer or women with ovarian cancer,” says Dr. AlHilli.
Advertisement
The most important lesson the researchers learned from their experience with this patient was the importance of multidisciplinary care coordination. “With a cancer diagnosis, things usually move quickly,” Dr. AlHilli notes. “When the patient is a young woman who wants fertility preservation, the gynecologic oncologist, gynecologist and reproduction endocrinologist must work together to ensure counseling can be delivered quickly, and appropriate options put into place without delay.”
Advertisement
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units