Dose-finding trial adds to evidence of efficacy
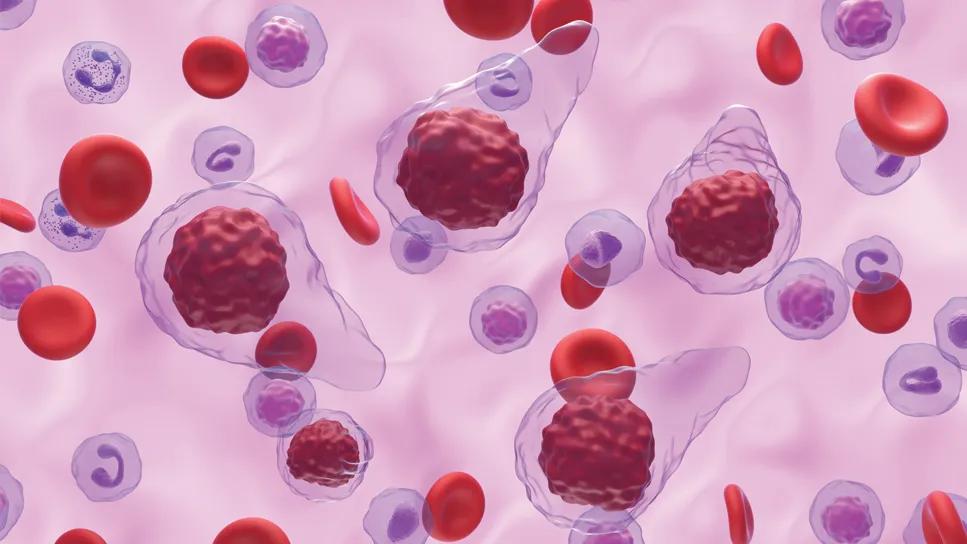
After a few uncertain years, the drug pacritinib may be headed towards FDA approval for the treatment of myelofibrosis, an uncommon type of bone marrow cancer that results in the formation of fibrous scar tissue and can lead to severe thrombocytopenia, anemia, enlarged spleen and liver. Final results of the latest pacritinib trial, PAC203, which are reported in Blood Advances, established the ideal dosing that is efficacious without causing unacceptable adverse events.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This is good news for the 26% of myelofibrosis patients with platelet counts below 50,000/µL, who have difficulty with treatment with ruxolitinib or fedratinib, JAK inhibitors approved to treat the disease. “This population has no approved therapy and, without treatment, has average survival of seven to 14 months,” says Aaron T. Gerds, MD, MS, a staff hematologist in the Cleveland Clinic Cancer Center’s Department of Hematology and Medical Oncology.
In 2016, the FDA placed a full clinical hold on pacritinib, an oral JAK2/IRAK1 inhibitor, due to concerns over excess deaths and cardiac and hemorrhagic complications in the preliminary results of the PERSIST-1 phase 3 study. This halted PERSIST-2, a second phase 3 study specifically enrolling patients with thrombocytopenia, resulting in incomplete data. After a review of the data from both PERSIST studies, the hold was released in 2017, which enabled further studies to be conducted.
The PERSIST-1 study demonstrated that pacritinib was well tolerated by myelofibrosis patients and more effective for reducing spleen volume and controlling symptoms than the best available treatment (BAT). PERSIST-2 showed that two dosing regimens of pacritinib (BID and QD) both led to greater spleen volume reduction (SVR) than BAT (which included ruxolitinib) for myelofibrosis patients with platelet counts of less than 100,000/μL. The side effects that occurred were common but controllable.
PAC203 was a randomized dose-finding study of pacritinib in patients with advanced myelofibrosis who are intolerant of or resistant to ruxolitinib. Of 161 patients, 73% were intolerant of and 76% had become resistant to ruxolitinib; 50% met criteria for both. Severe thrombocytopenia (platelet count 50 x 103/μL) was present in 44%. The study implemented strict risk mitigation measures.
Advertisement
Patients were randomized 1:1:1 to pacritinib 100 mg once per day, 100 mg twice per day or 200 mg twice per day. Pharmacokinetic and pharmacodynamic modeling based on all available data showed greatest SVR and total symptom score (TSS) reduction at 200 mg twice per day compared with lower doses. The rates of adverse events were lower than previously observed on the PERSIST-2 arm of 200 mg twice per day.
A substantial number of patients had high-risk molecular mutations, including a higher proportion with TP53 mutations than has been reported in other myelofibrosis cohorts, even those with previous ruxolitinib exposure (7.3% on PAC203 vs 1% to 4% previously reported). The majority of patients were anemic and thrombocytopenic, a profile characteristic of the myelodepletive myelofibrosis phenotype. The use of current first-line therapies for myelofibrosis, such as ruxolitinib and fedratinib, is limited in myelodepletive disease because these drugs can exacerbate cytopenias.
As observed in PERSIST-1 and PERSIST-2, patients with severe thrombocytopenia who were treated in PAC203 attained spleen and symptom responses despite previous exposure to ruxolitinib. Although the biologic basis of this well-documented observation is not fully understood, it is likely a function of both the kinase inhibition profile of pacritinib, which includes IRAK1, and differences in myelofibrosis biology in which thrombocytopenia and associated low JAK2 allele burden may represent a distinct myelofibrosis subgroup that is particularly responsive to pacritinib.
Advertisement
“Ultimately, in a high-risk population, we still see a response to pacritinib, with the higher dose having the most favorable efficacy. Pacritinib spares platelet production so it can improve symptoms without reducing platelet count,” says Dr. Gerds. “It worked in front-line and second-line settings.”
PAC203 paved the way for the PACIFICA trial, an ongoing randomized, controlled phase 3 study of pacritinib (200 mg twice per day) versus physician’s choice in patients with primary myelofibrosis, post-polycythemia vera myelofibrosis or post‑essential thrombocythemia myelofibrosis with severe thrombocytopenia (platelet count < 50,000/µL). physician’s choice treatments include: low-dose ruxolitinib, corticosteroids, hydroxyurea, thalidomide or lenalidomide.
At the same time, CTI Biopharma, the developer of pacritinib, has submitted a New Drug Application (NDA) to the FDA seeking approval of the drug as a treatment for myelofibrosis patients with severe thrombocytopenia (platelet counts less than 50 x 109/L). “It’s remarkable that an NDA is in process even before the trial is completed. If the drug is ultimately approved, it will go a long way to help a population that desperately needs a therapy that can treat the disease without excess bleeding,” says Dr. Gerds.
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists