Cleveland Clinic study finds superior overall survival for partial nephrectomy but cause still uncertain
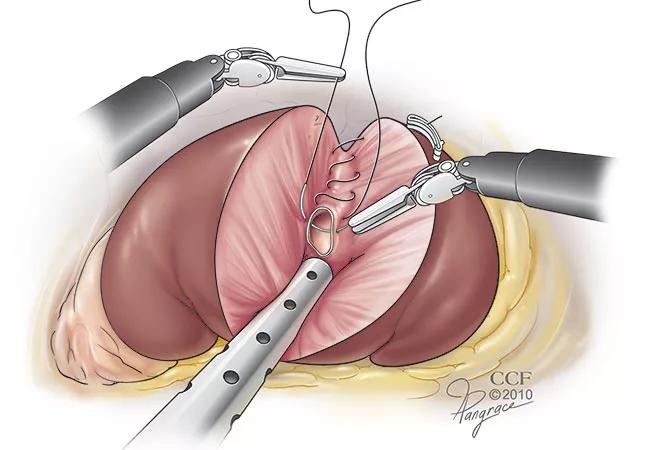
Over the past decade, partial nephrectomy (PN) has become the preferred surgical approach to treating localized renal cancer: It preserves more kidney function than radical nephrectomy (RN) and, according to most retrospective studies, offers better survival outcomes, even when elective. Selection bias, however, may influence the outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The only randomized trial of PN vs RN, which was conducted by the European Organisation for Research and Treatment of Cancer (EORTC 30904), did not find a survival benefit for PN, although RN resulted in a higher incidence of chronic kidney disease (CKD). Overall, high-level evidence on this key issue in renal cancer treatment is lacking.
Consequently, there is still controversy in the medical community concerning which procedure is preferable. “It is unclear where the boundary should be in deciding which procedure is best for the patient when there is a normal contralateral kidney,” says Steven C. Campbell, MD, PhD, urologic surgeon and a member of the Section of Urologic Oncology in Cleveland Clinic’s Glickman Urological and Kidney Institute.
To further investigate the outcomes of the two procedures, Cleveland Clinic Glickman Urological and Kidney Institute conducted a retrospective study of patients who underwent renal cancer surgery at the center. Nonrenal cancer-related mortality (NRCM) was the primary end point because it balances out oncological differences between the two cohorts (RN and PN) and more accurately reflects the impact of functional differences on survival.
The study is reported in The Journal of Urology.
The patient cohort included 3,133 patients age 18 or older without preexisting CKD, with a preoperative glomerular filtration rate (GFR) of 60 ml/minute/1.73 m2 or greater who had PN or RN performed at Cleveland Clinic from 1997 to 2008. The overall median age was 59 and the median preoperative GFR was 85 ml/minute/1.73 m2, which was identical in both cohorts.
Advertisement
Choice of procedure type (RN vs PN) was based on surgeon preference taking into account patient and tumor characteristics.
Patients were followed for a median time of 9.3 years. The new baseline GFR was 80 and 63 ml/minute/1.73 m2 after PN and RN respectively. The ten-year NRCM was 11.3% and 17.7% for PN and RN respectively. NRCM was similar in all patients who had a new baseline GFR of 45 ml/minute/1.73 m2 or greater. However, NRCM increased 50% or more in the 290 patients with a new baseline below this level.
In patients with a new baseline greater than 45 ml/minute/1.73 m2, the 10-year NRCM was still significantly improved after PN, 10.6% compared to 16.3% for RN. The functional outcome was higher with PN, with a median 95% preservation of global renal function compared to 74% for RN.
Most notably, the study found that in patients with a new baseline GFR greater than 45 ml/minute/1.73 m2, the functional dividend of PN, higher new baseline GFR, was not associated with survival on multivariable analysis while selection for PN vs RN maintained statistical significance. “This suggests classic selection bias. Since PN patients do not have better outcomes due to better kidney function, the most likely explanation is that they are healthier prior to treatment. Surgeons tend to perform RN on older, frailer patients who are less able to tolerate a more complex procedure,” says Dr. Campbell.
With better outcomes observed in patients with a GFR greater than 45 ml/minute/1.73 m2, achieving this level should be a goal of treatment; PN should be prioritized if needed to accomplish this. Surgeons can preoperatively estimate the final GFR with RN, based on a renal function scan for split renal function and presuming 10-20% compensatory hypertrophy following surgery. If the new baseline GFR is estimated to be less than 45 ml/minute/1.73 m2, PN is the best option.
Advertisement
The only way to resolve the PN/RN controversy, according to Dr. Campbell, is with another randomized clinical trial. Cleveland Clinic is strongly advocating for a trial, specifically for patients with clinical T1B/T2, and hopes one will be conducted in the near future.
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key