Combination therapy may help address underlying disease
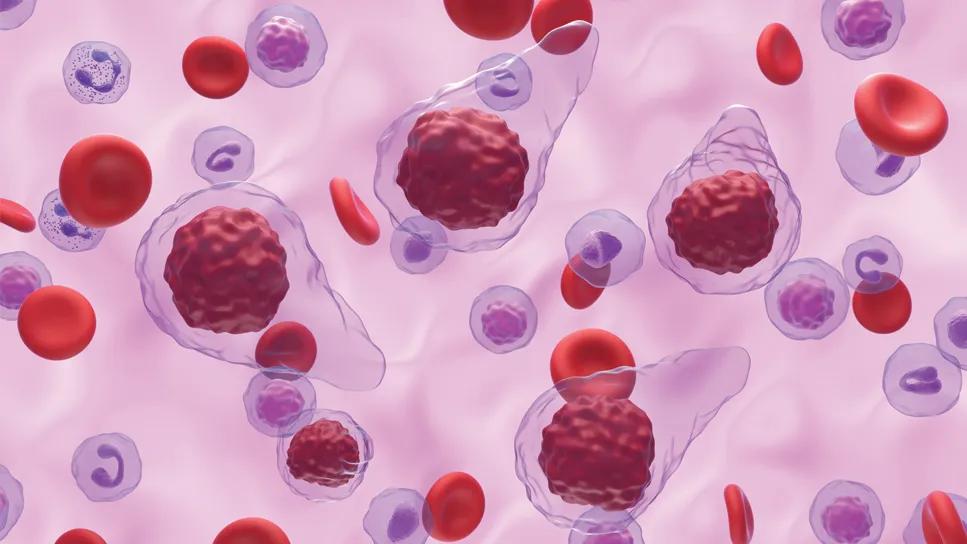
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/770733be-413b-4f01-8c82-dd945a083e76/treating-anemia-in-myelofribosis-1637356040)
Myelofibrosis cells
Upwards of 35-54% of patients newly diagnosed with myelofibrosis present with anemia, many of whom require transfusions. These days, there is no standardized approach to treating those patients. As new agents have emerged, clinicians are discovering how to individualize anemia therapy.
Amid rapid changes in the therapeutic landscape, Cleveland Clinic hematologists Akrita Jain and Aaron Gerds published a paper in the ASH publication Blood highlighting key treatment considerations.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Anemia is associated with lower survival rates in patients with myelofibrosis. In addition, the exhaustion that accompanies anemia contributes to a diminished quality of life.
Until a few years ago, clinicians had few options for addressing anemia beyond blood transfusions and supportive agents such as erythropoiesis stimulating agents. However, these did not address the underlying cause of the anemia, and they didn't contribute to improving patients' overall survival.
Today, there are several newer disease-modifying therapies available.
"Anemia can occur for multiple reasons," explains Akriti Jain, MD. “It could be caused by a production defect or it could be from blood loss in one shape or form. Patients need a comprehensive anemia workup that includes testing for all nutritional deficiencies that can lead to anemia."
The most common tests include iron, B12 and folate panels. Clinicians should also test for uncommon nutritional deficiencies, including copper, zinc, B1 and B6. Considering myelofibrosis as a disease state should also be part of the workup, as bone marrow scarring and inflammatory cytokines can lead to functional iron deficiency by increasing the hepcidin levels.
“While it's not essential to know exactly what is leading to the anemia, it's important to know what level of anemia the patient has, whether they’re symptomatic and if there are other concomitant deficiencies, so you can treat in an individualized manner,” says Dr. Jain.
Choosing the right therapeutic agent depends on many factors, such as whether the patient is presenting with anemia alone or if they have a constellation of myelofibrosis symptoms, such as fever, weight loss or abdominal discomfort. Symptoms can be evaluated using the Myeloproliferative Neoplasm Symptom Assessment Form (MPN-SAF). Understanding whether the anemia is caused by the disease or by medication can also help guide treatment decisions.
Disease-modifying therapies include the JAK inhibitor ruxolitinib, which has demonstrated overall survival benefits. "Ruxolitinib is the backbone of treatment but it's not appropriate for all situations," notes Dr. Jain. “It may be used in combination with other treatments or we may choose another option altogether."
If a patient has thrombocytopenia or low platelets along with anemia, pacritinib can be an option. If a patient has myelofibrosis symptoms and anemia, momelotinib may be considered. Also, the JAK inhibitor fedratinib could be used as second-line therapy for patients who don't respond to ruxolitinib.
Advertisement
It's not uncommon for patients who have started taking ruxolitinib for myelofibrosis to begin experiencing anemia. "The first inclination when this occurs may be to dose reduce, which can be appropriate, but we may tolerate a certain amount of anemia in some cases to achieve a spleen volume response or MPN symptom benefit,” says Dr. Jain.
Multiple studies demonstrated improved outcome among patients who received a 20mg dose for at least six months and experienced a decrease in spleen volume. The RR6 model can be used to predict survival in myelofibrosis based on a clinical response to ruxolitinib.
Clinicians are carefully watching trials of several potential new therapies, including:
• A phase 3 trial of the BET inhibitor pelabresib in combination with ruxolitinib. (At the ASH conference, researchers demonstrated the ability of this combination to decrease bone marrow fibrosis and inflammatory cytokines.)
• A phase 3 trial studying the addition of the p53 modulator navtemadlin for patients who had a suboptimal response to ruxolitinib. (This therapy may improve hematopoiesis and bone marrow function by reducing inflammation in the bone marrow.)
• A phase 1 trial studying the use of monoclonal antibodies that target and turn off the mutated CALR receptor.
As with most patients with myelofibrosis, those who present with anemia need to be monitored closely, with lab work every two to four weeks. The aim is to decrease or eliminate the need for transfusions if possible to improve patients’ quality of life and avoid iron overload and other complications.
As more new disease-modifying therapies become available, there will be more opportunities to help normalize bone marrow function and improve red blood cell production.
Advertisement
Advertisement
Combination therapy doubles the number of meaningful spleen volume responses over monotherapy
Approach resulted in transfusion independence and durable anemia response
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3
What’s coming up at ASH and beyond
Researchers Assess Real-Life Experiences of Patients Treated Outside of Clinical Trials
Early, individualized diagnosis and comprehensive management key to preserving fertility
Key considerations when diagnosing and managing severe hyponatremia