Two-drug therapy reduces progression in rare hereditary cancer syndrome
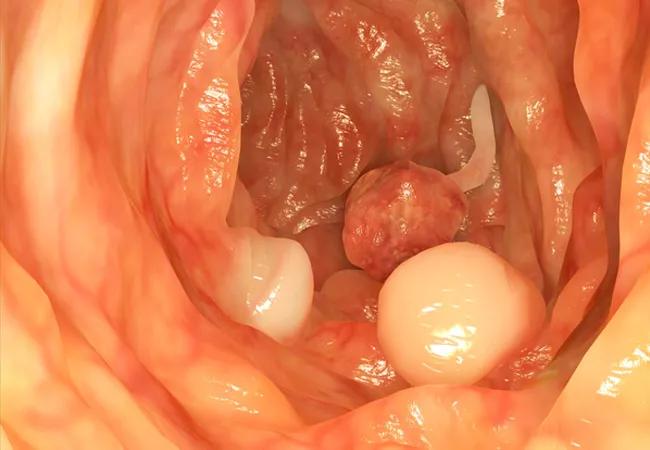
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/838f7312-2b48-4d33-ba38-01b0144006ac/19-DDI-238-Polyps-CQD-Hero_jpg)
19-DDI-238-Polyps-CQD-Hero
Results of a new phase 3 study led by Cleveland Clinic’s Carol Burke, MD, show promising results for a two-drug combination in reducing the need for surgery in patients with familial adenomatous polyposis (FAP). FAP is an inherited colorectal cancer (CRC) syndrome caused by a germline mutation in the adenomatous polyposis coli gene. Progression to CRC is inevitable in patients with FAP who have not undergone colectomy, with an average age of onset of 39.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Published in New England Journal of Medicine, the trial examined the safety and efficacy of sulindac or eflornithine alone versus both drugs in combination in patients with FAP. Eligible adults with FAP were randomized to eflornithine 750 mg, sulindac 150 mg or both once daily for up to 48 months.
“Hitting two different molecular pathways in FAP, we believed, would be more successful than targeting a single pathway to control FAP-associated polyposis,” says Dr. Burke.
The study was powered for a two-year event rate (polyp progression) in the combination arm of 30% versus a predicted 70% event rate in the monotherapy arms and included an analysis of polyp progression both in the duodenum and in the large intestine. When the results in both organs were examined, there was no significant difference between the effects on polyp progression of combination therapy or the individual drugs alone. The actual polyp progression rate at two years for the combination arm was 29%, but in the sulindac and eflornithine monotherapy arms, it was lower than predicted at 33% and 39%, respectively.
The most clinically meaningful findings were those resulting from the analysis of the lower intestinal tract. “The data showed that no patients in the combination arm with an intact colon or post-colectomy with an intact rectum or ileal pouch required surgery or excision of large polyps, while a significant number of patients in each of the monotherapy arms did,” says Dr. Burke, who is Vice Chairman of the Department of Gastroenterology and Hepatology, Director of the Center for Colon Polyp and Cancer Prevention and Head of the Section of Polyposis in the Sanford R. Weiss, MD, Center for Hereditary Colorectal Neoplasia. David Liska, MD, currently heads the center, which brings together experts from across disciplines to treat hereditary colorectal cancers.
Advertisement
In the patients who had not undergone colectomy, the lowest incidence of polyp progression was seen in those who received the sulindac/eflornithine combination, with hazard ratios of 0.30 (95% confidence interval [CI], 0.07 to 1.32) compared with sulindac alone and 0.20 (95% CI, 0.03 to 1.32) compared with eflornithine alone.
“I was disappointed to see that the combination did not impart a benefit in the duodenum, an organ that has limited treatment options for advanced duodenal polyposis control,” says Dr. Burke.
“Efficacy and safety were measured by the need for surgery or excision of large polyps, stage progression of duodenal polyposis or development of advanced neoplasia,” says Dr. Burke. “Assessment of time to first FAP-related event in the patient as a whole was a novel endpoint for chemoprevention studies.” Time-to-event prognosis was used to stratify the participants into one of three treatment arms: best (longest time to first FAP-related event), intermediate (duodenal polyposis) or worst (precolectomy).
In terms of safety, no statistically significant differences were seen in adverse events (AEs) between the study arms. In fact, the number of patients reporting grade 3 treatment-related or serious AEs was no higher in the combination arm than in the sulindac monotherapy arms.
“The data showing a decrease in the need for primary or secondary colorectal surgery over the time of the study are very compelling,” says Dr. Burke. “Sulindac monotherapy is already being used in selected patients with FAP. Based on our results, clinicians may want to incorporate the eflornithine/sulindac combination as a treatment strategy, if it receives approval from the US Food and Drug Administration (FDA).”
Advertisement
The trial’s sponsor will be working with the FDA on a pathway to approval for the two-drug combination, but they are not planning any systematic follow-up of the participants. Most of the patients, however, will be monitored at the Sanford R. Weiss, MD, Center for Hereditary Colorectal Neoplasia on at least an annual basis or by staff of the David G. Jagelman Inherited Colorectal Registries for any off-therapy rebound in polyp burden.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches