Time-lapse microscopy allows more in-depth analysis
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0f39262c-b12a-4fb8-a503-9fa9d5727698/15-URL-079-Sabanegh-Hero-Image-690x380pxl-jpg)
18-OBG-1363-DesaiSpermFertEgg-650×450
Sperm DNA fragmentation has been suggested to be a contributor to male infertility and lower pregnancy outcomes. However, the degree to which DNA fragmentation influences outcomes in in vitro fertilization (IVF) intracytoplasmic sperm injection (ICSI) cycles is still controversial. Integration of time-lapse microscopy (TLM) into IVF labs allows more in-depth analysis of embryo developmental kinetics than was previously possible with conventional microscopy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A Cleveland Clinic study examined sperm DNA fragmentation and its relationship to embryo morphokinetics, multinucleation and cleavage anomalies,” explains Nina Desai, PhD, HCLD, Fertility Center Lab Director, Ob/Gyn & Women’s Health Institute, who co-authored a paper on the topic with IVF Technologist Stephanie Ploskonka, MS. The paper was published in Fertility and Sterility Journal in September 2018 and was presented today at the American Society for Reproduction Medicine Scientific Congress & Expo.
The study encompassed 77 couples undergoing IVF. Sperm specimens were prepared for ICSI using density gradient centrifugation. Mature oocytes were fertilized by ICSI and immature oocytes were incubated overnight with sperm. Normally fertilized oocytes were cultured in the EmbryoScope time lapse chamber. Timing of specific events from the point of insemination was determined using time lapse (TL) imaging and expressed in hours.
The following kinetic markers were assessed: time to syngamy (t-syn), time to 2c (t2), 3c (t3), 4c (t4), 5c (t5), 8c (t8), morula (Mor-t), start of blastulation (tSB), blastocyst (BL-t), and expanded blastocyst (EBL-t). Durations of the second (cc2) and third (cc3) cell cycles as well as time to complete synchronous divisions s2 and s3 were calculated.
Embryos were also observed for presence or multinucleation and cleavage anomalies. Sperm DNA fragmentation testing was performed on an aliquot of the unused ICSI sperm preparation using the Halosperm kit (HaloTech/Spectrum Technologies). The kit enabled microscopic detection of sperm chromatins dispersion.
Advertisement
Sperm were embedded in agarose coated slides and exposed to acid denaturation and a lysis buffer. Following alcohol dehydration and staining with DiffQuik, slides were examined to detect presence of halos surrounding sperm. Sperm cells with large/medium sized halos characteristic of dispersed DNA loops were considered to have intact DNA. Sperm with small, degraded or absent halos were considered to have fragmented DNA. Cases were divided according to % DF in ICSI specimens. Morphokinetic parameters were compared. P value of <0.05 were considered to be statistically significant.
Embryos created from ICSI with sperm samples showing high levels of DNA fragmentation showed more early-dysmorphisms like multinucleation and chaotic cell division. Their developmental kinetics also were significantly different. High sperm DNA fragmentation was associated with a lower percentage of embryos, forming morula and developing to the expanded blastocyst stage.
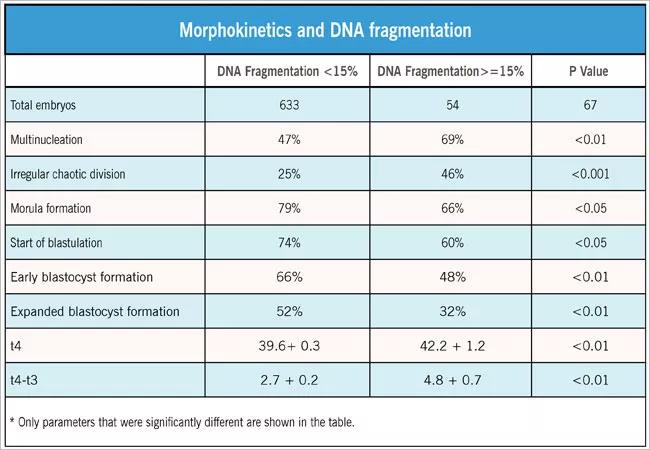
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/11e14cb4-2017-4c86-a9dc-5a5bf717ec87/18-OBG-1363-DesaiSpermChrt-650x450_jpg)
The Halosperm kit provided an easy, inexpensive means to assay DNA fragmentation.
High DNA fragmentation is one marker that may explain why a patient is not making good quality embryos.
Further study is needed on the association between sperm DNA fragmentation and embryo quality markers made possible through time lapse imaging systems.
Advertisement
Advertisement
A Q&A with Cleveland Clinic’s board-certified pediatric and adolescent gynecologist
Increasing uptake remains a challenge
Multidisciplinary teams work together in in-situ scenarios
Uterine transposition cleared the field for radiation therapy
ACOG-informed guidance considers mothers and babies
Prolapse surgery need not automatically mean hysterectomy
Artesunate ointment shows promise as a non-surgical alternative
New guidelines update recommendations