Referral network for inherited cancer syndromes
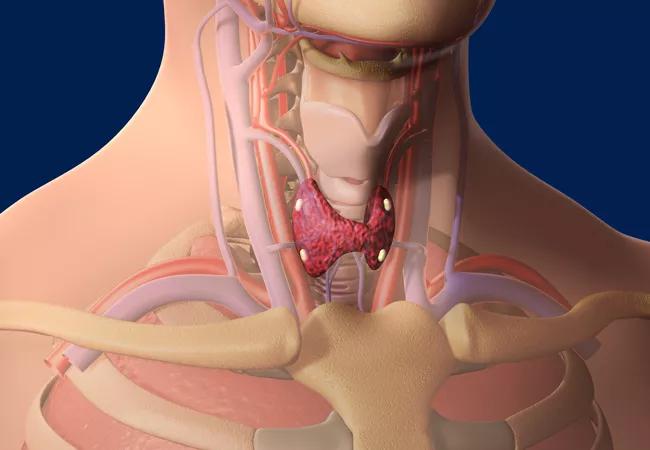
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e5982f51-d198-477d-aa18-4c6dac5c2709/thyroid_650x450_jpg)
thyroid_650x450
By Rosemarie Metzger, MD, MPH
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Significant advancement has occurred in the field of hereditary thyroid cancer syndromes. An important realization is that these conditions are not as rare or as difficult to recognize as previously thought.
While multiple endocrine neoplasia type II (MEN2) is well known to be associated with medullary thyroid cancer (MTC), there are other inherited cancer syndromes whose associations with thyroid cancer might be less well known — including Cowden syndrome (CS) and familial adenomatous polyposis (FAP).
At Cleveland Clinic, endocrinologists, endocrine surgeons, gastroenterologists and colorectal surgeons work collaboratively with geneticists, researchers and other clinicians to foster a referral network for thyroid screening in patients with inherited cancer syndromes.
CS is associated with a known genetic basis, although its diagnosis can be easily missed. CS is a rare, dominantly heritable disorder in which the clinical findings can be subtle — until the genetic basis was determined, they were the only way to diagnose CS.
CS is now known to be one of several genetic syndromes characterized by germline mutations of the tumor suppressor PTEN. These mutations predispose patients to benign hamartomatous changes as well as malignant transformation of epithelial tissues, including breast, thyroid, kidney, intestine and endometrium.
This knowledge has led to an evolution in both the diagnosis of CS and the understanding of its associated disease spectrum, which has affected management and therapy decisions.
Advertisement
Recognizing individuals with CS is especially important given the frequency of associated cancer and the inherent implications for surveillance. In PTEN mut+ patients, thyroid cancer has the earliest onset and the second highest lifetime risk (35 to 38 percent), second only to breast cancer.
The elevated risk of thyroid cancer from birth is of particular importance and has guided updates to screening recommendations. Specifically, thyroid ultrasound should be performed at the time of CS diagnosis and annually thereafter, even in the pediatric population. For that reason, every patient seen at Cleveland Clinic in our PTEN Cowden Clinic is referred for thyroid screening by one of our endocrine surgeons. Screening includes a thyroid-focused history and physical exam with neck ultrasound.
Given the association of PTEN mutation with both benign and malignant transformation, a high prevalence and early onset of both benign and malignant thyroid disease has been identified. Goiter has been found in more than 50 percent of patients screened, and Hashimoto’s thyroiditis in almost 50 percent. Nearly half of those presenting for initial screening have had indications for fine-needle aspiration biopsy.
The PTEN Cowden Clinic is run by Charis Eng, MD, PhD, chair and founding director of the Cleveland Clinic Genomic Medicine Institute, who led the research team that discovered the causative relationship between the PTEN gene and Cowden syndrome.
Much like Cowden syndrome, FAP has been associated with both benign and malignant transformation of the thyroid. FAP is an autosomal dominant disorder due to germline APC mutation and is characterized by multiple colorectal polyps with a nearly 100 percent lifetime risk of developing colorectal cancer if left untreated. It is now widely recognized to be associated with extracolonic cancers as well.
Advertisement
Recent investigation into FAP has revealed a higher prevalence (2 to 5 percent) of thyroid cancer than previously expected, which has influenced recommendations for screening and management.
A prospective thyroid screening trial for FAP patients undergoing annual gastrointestinal (GI) surveillance at Cleveland Clinic found thyroid cancer in 2.6 percent of patients who had an initial thyroid screening. Given that benign nodularity was identified in a 17-year-old patient with FAP, the suggested age of screening initiation is 16 years.
We have now adopted a more formal screening program in which all patients with FAP who present for their GI screening in the GI or colorectal surgery departments have a coordinated visit scheduled for thyroid screening by an endocrine surgeon. Thyroid cancer in FAP patients detected by ultrasonographic screening is smaller and associated with fewer surgical complications, fewer recurrences and fewer cancer-related deaths.
As our understanding of both CS and FAP and their links to thyroid cancer continues to expand, it’s important to update screening recommendations accordingly so that earlier diagnosis and intervention can occur.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches