A new study explores survival outcomes based on treatment modality
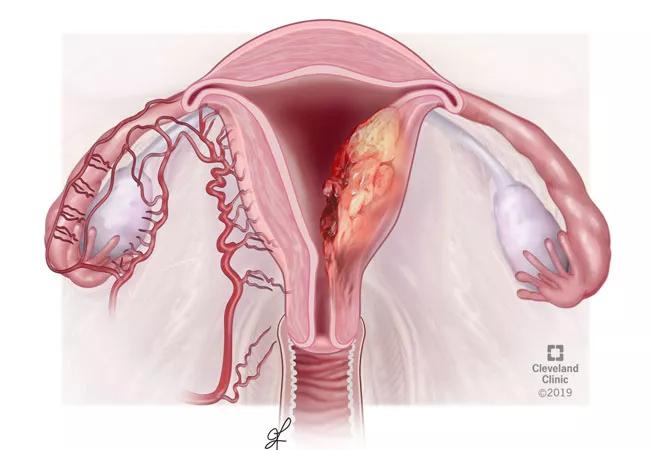
Treatment modality is a significant predictor of overall survival for women with advanced endometrial cancer (EC), according to a recent Cleveland Clinic study. The findings suggest that when possible, physicians should include surgery in treatment planning for women with advanced EC, says Mariam AlHilli, MD, a gynecologic oncologist and senior author of the study.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In the analysis, which was published in Gynecologic Oncology, physician-researchers investigated the impact of neoadjuvant chemotherapy (NACT) on survival in women with stage III or IV endometrial cancer.
“In women with a newly diagnosed advanced stage endometrial cancer, primary cytoreductive surgery is associated with superior oncologic outcomes and is recommended for first-line management, if feasible. However, primary surgery may not be appropriate for all women diagnosed with advanced endometrial cancer due to disease burden, medical comorbidities or performance status. In these patients, evidence is limited to guide treatment decisions. We designed a study to assess how treatment paradigm impacts survival in women diagnosed with advanced endometrial cancer,” notes Laura Chambers, MD, first author on the study.
The Cleveland Clinic team used the National Cancer Database (NCDB) to determine differences in overall survival in patients with stage III/IV endometrial cancer. Included patients (N = 48,179) received one of three different treatment modalities from 2004-2015, namely chemotherapy (CT) alone (N = 5,531, 11.5%), NACT and interval debulking surgery (IDS) (N = 2,614, 5.4%), and primary cytoreductive surgery (PCS) and chemotherapy (N = 40,034, 83.1%).
“The NCDB includes a heterogeneous group of patients, with large variability in demographic characteristics and oncology practice patterns,” states Dr. AlHilli. “For most women with a new diagnosis of advanced endometrial cancer, the best outcomes are with primary surgery followed by chemotherapy.”
Advertisement
Regardless of stage or histology, in women with advanced endometrial cancer, PCS + CT was associated with improved overall survival (60.9 months) compared with NACT + IDS (25.1 months) and CT alone (11.1 months). NACT + IDS was also associated with better overall survival in stage III type I and all stage IV EC compared with CT alone. The role of PCS in women with stage III disease and type II histology was affirmed, and there was no survival difference in those who received CT or NACT + IDS.
Even in women with stage IV disease, who tend to have a poor prognosis, CT alone was associated with worse survival than either PCS + CT or NACT + IDS. In patients with stage IV type I and I disease, PCS + CT was better than NACT + IDS. However, this finding differs from previous studies that found no difference OS difference in women undergoing either NACT + IDS or PC + IDC. In this population, surgical treatment should be individualized for each patient.
Additional factors that predicted worse OS were advanced age, African American race, stage IV disease, higher Charlson-Deyo Score, increased tumor grade and type II histology.
For various reasons, 5,356 patients (11.1%) did not undergo surgery. Rationale for this included: surgery was not part of the primary treatment plan (N = 4493, 83.9%), surgery was contraindicated for patient-related factors such as medical comorbidities and oncologic characteristics (N = 470, 8.8%), patient refusal (N = 64, 1.4%), patient death (N = 52, 1.0%) and unknown (N = 198, 3.7%).
Advertisement
The results of this study suggest survival benefits of PCS in this population (60.9 months versus 11.1 months for chemotherapy alone). “We suspected surgery would have survival benefits, but were surprised by the extent of the differences in survival outcomes between these treatment modalities. In cases involving extensive cancer, surgeons may want to refer to a tertiary care center, such as Cleveland Clinic, with more experience in such aggressive surgeries,” concludes Dr. Chambers.
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists