Negative affect reported in several sexuality-related functions at two years
For men with early stage prostate cancer, adding neoadjuvant androgen deprivation therapy (NADT) to external beam radiation therapy (EBRT) or brachytherapy (BT) led to significantly worse health-related quality of life (HRQOL) in three measures, according to a study in the International Journal of Radiation Oncology. The measures — the ability to reach orgasm, quality of erections and ability to function sexually — were identified from patient-reported outcomes gathered over two years by members of the Prostate Cancer Outcomes and Satisfaction with Treatment Quality Assessment Consortium, the multicenter group that sponsored the paper.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The results provide useful insights for clinicians, says Eric A. Klein, MD, Chairman, Glickman Urological & Kidney Institute, and a study co-author. The most important insight is that while NADT and EBRT improve survival in intermediate- and high-risk patients, these treatments can decrease a number of quality-of-life parameters. NADT is not known to favorably influence outcome after BT. Therefore, it is vital that physicians provide pretreatment counseling about the effects these treatments may have on quality of life.
“In this study, the biggest quantifiable difference in HRQOL had to do with NADT, rather than which radiation modality was used,” states Cleveland Clinic radiation oncologist Jay Ciezki, MD, an author on the paper.
In the study, reporting from nine U.S. academic centers, 573 patients whose prostate cancer was newly diagnosed were evaluated using a prostate cancer-specific 26-item questionnaire at 2, 6, 12 and 24 months after the start of NADT. The researchers looked at six questions in the survey’s sexual domain and five in the vitality/hormonal domain.
In general, the patients who received NADT had worse overall cancer severity based on several measures, such as prostate specific antigen (PSA) levels, Gleason scores and T stages. Compared with patients who received ERBT alone, patients who received EBRT and NADT had worse HRQOL, as measured by the frequency of erections, quality of erections, ability to have erections, ability to reach orgasm, ability to function sexually and lack of energy.
Advertisement
However, when comparing the baseline versus 24-month outcomes, only the differences in the ability to reach an orgasm, quality of an erection and ability to function sexually were statistically significant. Interestingly, comparing six months to 24 months, the ability to have an erection, ability to reach orgasm and the frequency of erections did show statistical improvements. The authors noted this could be helpful for counseling at the six-month follow-up visit.
Because multiple studies show that adding short- and long-term ADT to radiation therapy in intermediate- and high-risk prostate cancer improves overall and cancer-specific survival, the authors were reassured by study findings that patients were not experiencing worse symptoms at 24 months for most of the sexual and hormone/vitality questions. However, they did note the necessity of pretreatment counseling on HRQOL effect of NADT and ERBT.
“The significance of difference in HRQOL in these three measures opens a door for better conversations with patients,” Dr. Klein notes.
“The evidence shows there’s not much difference in cure rates between standard treatments (ERBT or BT),” Dr. Klein says, “so when a patient asks what is the best treatment, or which treatment has the best cure rate or has the fewest side effects, we have to consider what’s important to this patient.” It is important for the patient to know that in certain types of prostate cancer, such as high-risk prostate cancer, NADT is required if EBRT is used. But NADT is not required if BT is used.
Advertisement
“Everything has a price,” Dr. Klein continues. “The question we have to ask each patient is ‘what quality of life do you want to have?’”
To stimulate conversations that give patients the information they need to make their own benefit-risk calculation, the researchers designed special graphics meant to be used during consultations for patient education, Dr. Ciezki says. The graphics allow patients to visualize differences in outcomes. Figure 1 is an example.
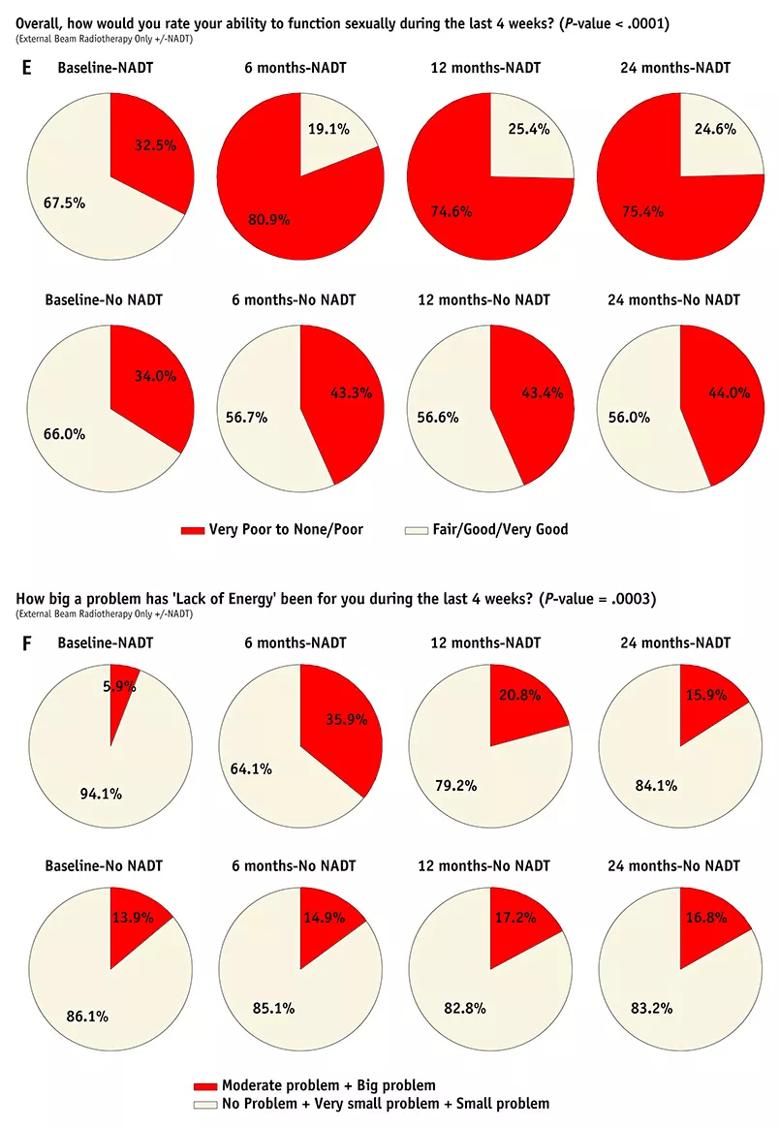
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/55067a65-efaf-4e91-8aca-f146fb631121/805x-Inset-Klein-Prostate-Cancer-Study_jpg)
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors