Retrospective study results underscore the need for colonoscopy in symptomatic people under age 50
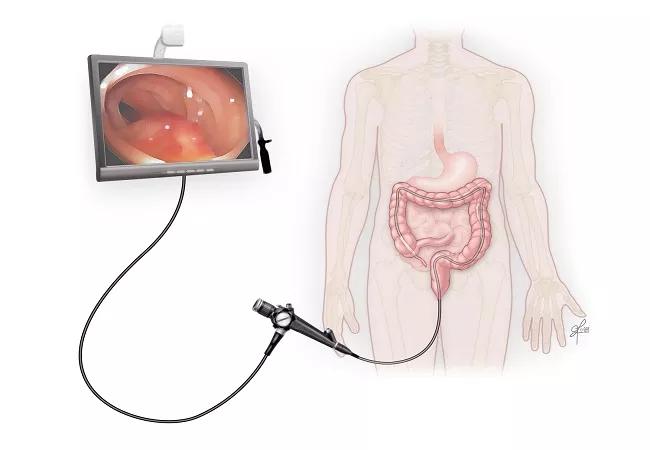
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b6cb2b51-e639-4d4d-8db9-198a643472ab/22-DDI-2861960-Young-onset-CRC-hero-image-650x450-1_jpeg)
22-DDI-2861960 Young onset CRC hero image 650×450
Diagnostic colonoscopy is warranted in adults younger than age 50 with classic “alarm” symptoms for colorectal cancer, based on the results of a retrospective study by Cleveland Clinic researchers presented at the 2022 American Society for Colorectal Surgery annual scientific meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Although the study found that the incidence of invasive adenocarcinoma was low among young symptomatic adults undergoing diagnostic colonoscopy, the prevalence of advanced neoplasia in patients with bleeding or weight loss exceeded 3%. That is comparable with the advanced neoplasia prevalence in high-risk adults aged 40-49 undergoing screening colonoscopy due to a family history.
“Our hypothesis was confirmed that there would be positive findings related to cancerous or precancerous lesions in younger patients with symptoms who underwent colonoscopy,” says colorectal surgeon David Liska, MD, who conducted the study along with colleagues, including Cleveland Clinic colorectal surgery fellow Tara Russell MD, PhD, MPH. “It’s important that these individuals be evaluated rather than clinicians assuming that, because of their young age, there is no risk for cancer.”
In 2021, the U.S. Preventive Services Task Force endorsed screening for colorectal cancer in anyone without risk factors for the disease beginning at age 45, five years sooner than the previous guidance recommended. The action was in response to the increasing incidence of colorectal cancer in adults younger than 50 since the mid-1990s.
With this new analysis, the Cleveland Clinic researchers hoped to help address the paucity of data on the frequency of neoplastic lesions in symptomatic young adults undergoing diagnostic colonoscopy.
Data from almost 33,000 adult patients aged 18 to 49 who had undergone diagnostic colonoscopy from 2011 to 2021 at Cleveland Clinic and affiliate community sites were included in the study. The majority of participants (69%) were white, 14.9% were Black and 9.6% were Hispanic. Nearly two-thirds of the patients (60.6%) were female and 39.4% were male.
Advertisement
The authors excluded patients who had undergone high-risk screening because of a family history of polyposis or cancer, surveillance because of a personal history of polyps or cancer, or evaluation for known inflammatory bowel disease.
Descriptive statistics were used to analyze indications for colonoscopy and pathologic findings. Odds of a positive finding were assessed with univariate analysis.
Of the 49,348 young adults who underwent colonoscopy during the 10-year study period, 32,649 (66.0%) had diagnostic examinations. The most common indications for those tests were a change in bowel habits (37.2%), bleeding (31.1%) and pain (17.4%).
“We used a really large database to identify patients at average risk for colorectal cancer other than their symptoms,” says Dr. Liska. “We were not, however, able to accurately assess whether these individuals had a family history of polyps or of colorectal cancer because that was not reported by the physicians who performed the colonoscopies.” Colonoscopy was considered positive if a patient was found to have adenomatous or serrated lesions other than hyperplastic polyps that measured < 10 mm. Neoplasia was considered advanced if a patient had an advanced adenoma (high-grade dysplasia, ≥ 25% villous component or ≥10-mm diameter), advanced serrated lesions (dysplasia or ≥ 10-mm diameter) or invasive adenocarcinoma.
Colonoscopy results were positive for neoplasia in 9.3% of patients who underwent diagnostic testing. In this diagnostic colonoscopy cohort, 2.1% were found to have advanced neoplasia and 0.04% had invasive adenocarcinoma. In other studies, CRC incidence has been reported to be ~ 0.5%.
Advertisement
Says Dr. Liska, “The incidence of cancer was lower than we anticipated, but there were approximately 700 patients in our study who were found to have advanced precancerous lesions. Had they not been screened with colonoscopy, the lesions potentially could have developed into cancer within the next few years.”
The median age of participants with advanced neoplasia was 45 (range 31 to 49 years). With increasing age, the prevalence of both a positive finding and detection of advanced neoplasia increased (P <0.001 for both models and individual covariates).
Positive findings or advanced neoplasia was most prevalent in patients who had been referred for colonoscopy because of bleeding, anemia, weight loss and abdominal mass. Race/ethnicity was not significantly correlated with prevalence of advanced neoplasia. During the decade covered by the study period, the number of positive findings and the number of cases of advanced neoplasia significantly increased year over year (P <0.05).
The next step for the researchers is to try to risk-stratify young patients with symptoms suggestive of colorectal cancer. Says Dr. Liska, “Maybe by taking more in-depth histories from some of these individuals, including family history and environmental exposures, we can identify those who are most likely to benefit from earlier colonoscopy.” Another challenge is determining what is driving the increase in colorectal cancer incidence in younger people. At Cleveland Clinic, “we’re pursuing a comprehensive analysis as a way to compare young people with and without colorectal cancer,” says Dr. Liska. “Our aim is to try to identify genes, microbiome features or an immune phenotype that may be predictive of higher risk for the disease.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches