Research shows promise for use in therapeutic settings to manage depression, PTSD, anxiety and more
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2243576/13534510)
Psychedelic drugs have reemerged in recent years as a promising treatment for a variety of behavioral health diagnoses, such as depression, post-traumatic stress disorder and generalized anxiety disorder.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“If patients go into the psychedelic experience with therapeutic intent and in a therapeutic setting, they can get benefits that may last for a year or even longer in some cases,” says Brian Barnett, MD, a psychiatrist in Cleveland Clinic’s Center for Behavioral Health.
Dr. Barnett discusses the current state of psychedelics research and what’s next for the field in the latest episode of Cleveland Clinic’s Neuro Pathways podcast. He covers:
Click the podcast player above to listen to the 28-minute episode now, or read on for a short edited excerpt. Check out more Neuro Pathways episodes at clevelandclinic.org/neuropodcast or wherever you get your podcasts. This activity has been approved for AMA PRA Category 1 Credit™. After listening to the podcast, you can claim your credit here.
Podcast host Glen Stevens, DO, PhD: How well do we understand the mechanism of action of these drugs?
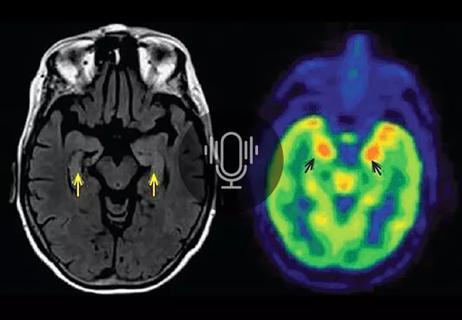
Dr. Barnett:In psychiatry in general, we don’t know a lot about how many of our treatments work. We have inklings here and there from different types of studies, but it looks like the primary mechanism at the neuronal level is that psychedelics activate the serotonin 2A pathway, so 5-HT2A. That pathway is involved in a number of areas — including learning, memory, pain perception and the sleep-wake cycle — but those receptors are most concentrated in what are called the higher-order association areas of the brain.
Advertisement
Those are the parts of the brain that integrate incoming sensory information, and it looks like psychedelics really allow more sensory input to enter the brain. They peel back the thalamus’s control over sensory input data, allowing more sensory data to come in, which overloads the brain and causes different areas that normally don’t talk to each other to communicate and connect. That is why people sometimes can get what’s called synesthesia when they take a psychedelic — experiencing sound as colors and things like that.
And from a different perspective, it appears that taking a psychedelic induces pretty long-lasting periods of neuroplasticity, where the brain is more flexible. During these periods, the brain is better able to reorganize synaptic connections, allowing a person to really adjust their perspective on things, see life from a different point of view, learn new ways of coping with stress. This is why we think that the period of several weeks afterward — maybe even several months — is when a lot of the therapeutic benefit comes, because patients can really engage in therapy at that point, and therapy can be catalyzed.
Advertisement
Advertisement

New research focuses on tumorigenic aspects of communication among brain cells
Evidence hints that chronic neuroinflammation might stem from a CNS-directed autoimmune response

Insights on leveraging collaboration and advocacy to develop and conduct needed trials
Comprehensive evaluation and keen clinical judgment are key in suspected cases

Why we’ve launched a targeted mentorship program and new dedicated funding awards

Planning continues with critical, patient-focused input from nursing teams

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Advances in genomics, spinal fluid analysis, wearable-based patient monitoring and more