Rate is lower with tunneled intravenous catheters
Patients with inflammatory bowel disease (IBD) who received home parenteral nutrition (HPN) via tunneled catheters had a lower risk of deep vein thrombosis (DVT) than patients whose HPN was delivered via peripherally inserted catheters (PICCs), according to a study presented at the American College of Gastroenterology 2020 Annual Meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Patients with IBD are at a higher risk of DVT than the general population,” says Mohamed Tausif Siddiqui, MD, fellow in the Department of Gastroenterology, Hepatology and Nutrition in Cleveland Clinic’s Digestive Disease & Surgery Institute, and presenter of the study. “Add in catheters for parenteral nutrition, and the risk increases even more. We wanted to investigate whether a particular type of catheter was safer for these patients.”
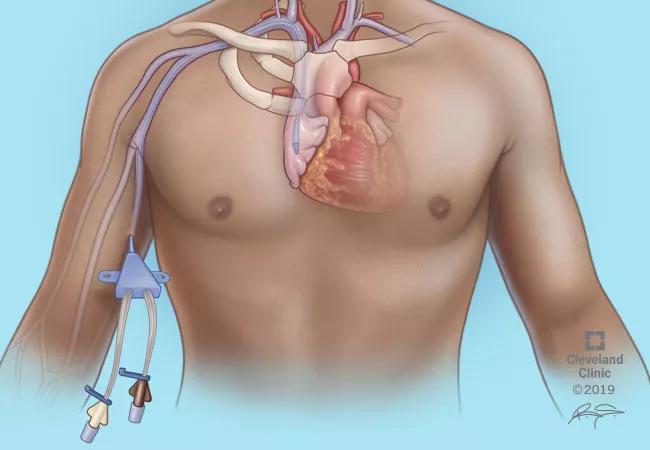
The team conducted a retrospective analysis of patients with ulcerative colitis and Crohn’s disease who received HPN from 2013 to 2019. A total of 407 patients and 744 catheter placements with a total duration of 317,777 days were analyzed. PICCs were placed in 205 (28%) of episodes, and the rest had tunneled catheters, which were also used for significantly longer periods compared with PICCs.
The overall rate of catheter-associated DVT was 4.4%. The study noted that the rate of catheter-associated DVT was 5.4% in patients with PICC lines compared with 4.1 % in those with tunneled catheters. When reviewing the rates by catheter days, PICCs had twice the rate of DVT compared with tunneled catheters (0.16 vs. 0.08 per 1000 catheter days, respectively). Since the tunneled catheters were used for significantly longer periods, the research team conducted a weighted analysis of the data. They used catheter days as weight for each episode and calculated an odds ratio (OR), which demonstrated that DVT risk was significantly higher with the use of PICCs (OR 3.665, 95% CI 3.516-3.820, P < 0.05).
Advertisement
“The data confirms our choice at Cleveland Clinic to use tunneled central lines for the majority of our IBD patients on home parenteral nutrition, especially when the duration of therapy is greater than four to six weeks,” says Donald Kirby, MD, Director of Cleveland Clinic’s Center for Human Nutrition. “PICCs are placed into smaller lumen veins compared with tunneled catheters, and thereby should be at higher risk of thrombosis. It has been our team’s long-term goal to minimize the potential complications that these patients experience.“
Cleveland Clinic’s Center for Human Nutrition enables the comprehensive evaluation, education and treatment of patients with disease-related nutrition problems. This innovative approach allows registered dietitians, dietetic technicians, nurses, pharmacists, physicians and surgeons to provide individualized plans for both adults and pediatric patients with specialized nutrition needs. The center focuses on three distinct areas: nutrition therapy, nutrition support and intestinal rehabilitation.
Extensive collaboration between the center and the IBD medical home led by Department Chair Miguel Regueiro, MD, was key to this research. “This research demonstrates our focus on whole-person care,” he says. “Patients in our IBD medical home get a one-stop shop for all kinds of expertise, including the Center for Human Nutrition, all led by their gastroenterologist.” Read more about the IBD medical home here.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years