New navigation technology helps surgeons go beyond what their eyes can see.

As a urology fellow at Cleveland Clinic, Jihad Kaouk, MD, FACS, FRCS (U’02) witnessed the birth of a new field of medicine. “I completed a fellowship in minimally invasive surgery just when robotics was introduced,” he says. “I was lucky to be in the right place at the right time.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Today, he is Director of Cleveland Clinic’s Center for Robotic and Image Guided Surgery at the Glickman Urological & Kidney Institute, Institute Vice Chair for Surgical Innovations, and holds the Zegarac-Pollock Endowed Chair in Laparoscopic and Robotic Surgery. In all of these roles, Dr. Kaouk contributes to innovation and growth in the field.
When introduced in 2002, robotics was intended for cardiothoracic surgery, he says. “But it was very difficult to do. Some surgeons, and I was one of them, decided to start exploring the robot for urological procedures.”
Once the FDA approved robotics for prostate surgery that same year, Dr. Kaouk began using the technology for parts of the procedure. Over time, he says, it became the standard for prostate cancer surgery.
“There was a huge shift from open and laparoscopic to robotic,” he says. “Now, 98 percent of prostate cancer glands are removed with the robot. It allows for magnified vision – up to 10 times – shines a powerful light deep into the pelvis, and the instruments articulate, so that you can get the exact angle better than in laparoscopy, in which the instruments are rigid.”
Applications expanded, and robotic surgery also became the standard for kidney and bladder cancer. “Patients benefit from quicker recovery, smaller incisions and less pain,” he says.
Dr. Kaouk says he was inspired to look for the most effective approaches when he studied with Andrew Novick, MD. “He proved that you don’t need to remove the entire kidney, just the bad part, and that will be as effective.” He also was influenced by mentor and laparoscopic surgery pioneer Inderbir Gill, MD.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/40baca92-f687-4753-94c3-67e536d7f1d6/Figure-2-2-1024x1024_jpg)
Intraoperative Footage of Operating Room Setup During Robotic Single Port Surgery
In the past decade, Dr. Kaouk has performed groundbreaking surgeries, including the first robotic single port surgery through the belly button in 2008, and the first completely transvaginal kidney removal in 2009, which allowed patients to be discharged within a day of surgery. He has one of the largest experiences in robotic surgery in the country, with more than 1,200 robotic radical prostatectomy and 500 robotic partial nephrectomy in the past decade. He also patented a device for radiofrequency cauterization and extraction of tissue, used mainly in partial nephrectomy.
Still, he is always seeking to do more.
“In 2007, I started thinking, ‘how can we further minimize ‘minimally assisted surgery?’” he says. “A robot requires five small cuts, but I wanted fewer. I thought about single-port surgery, with one small cut.”
A robot resembling a canula became available, through which another canula and three instruments can be placed and spread apart to perform procedures. “I worked with the engineers who developed this robot in the lab, and we did our initial clinical work in Europe before the FDA approved it here. When it became FDA-approved in 2008, we were the first in the world to get the robot on our Cleveland Clinic main campus.”
These procedures have been upgraded, he says. “Robotic surgery for prostate cancer leads to minimal blood loss and quicker recovery. Now, we do it in one incision, 2 inches or an inch-and-a-half, just below the belly button, with no other cuts at all, and we stay extraperitoneal. We don’t see or touch the bowel. We have same-day surgery for about 90 percent of the patients. We’ve operated on 200 patients since this started less than two years ago.”
Advertisement
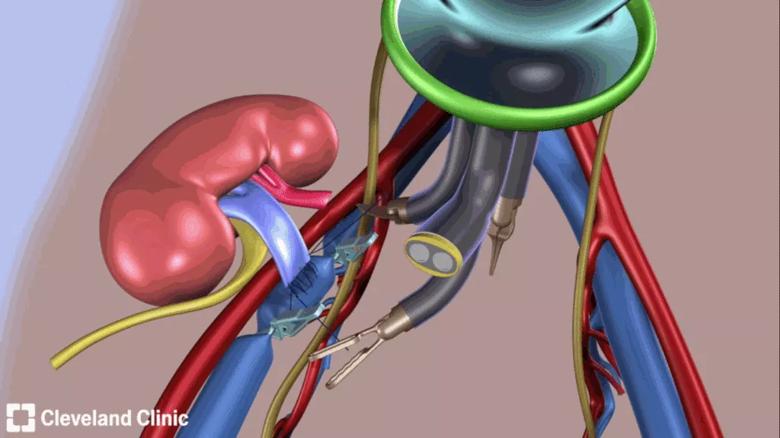
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/13283ead-c7ca-42bf-9023-c803796792df/Figure-1-1024x575_gif)
Single Port Robotic Extraperitoneal Kidney Transplantation
Single-port surgery is used in partial nephrectomy for kidney cancer, cystectomy for bladder cancer, and, for the first time a few months ago, in kidney transplants. “We went through a single port, one cut below the belly button,” Dr. Kaouk says. “We’ve had excellent success, and it’s also same-day surgery. We first did the transplant inter-abdominally, but refined the technique, and it’s now extraperitoneal. We just work in the region where we need to be.”
Early on, the concept of minimally invasive surgery focused on performing the task effectively. “Not much thought was given to collateral damage based on the size of the incision,” he says. “Now, we want to be true minimalists.” With the advent of natural orifice surgery – the mouth, anal area, belly button or transvaginal – requiring no cuts at all, Dr. Kaouk says he thinks surgery has been minimized as much as possible.
So, what is his next logical step? Rethink the robot.
In his Biomedical Engineering Department, Dr. Kaouk and five engineers are working on robotic automation. “Why replicate human moves when humans have limitations?” he says. Pilot studies are testing segments of the surgery in which a robot can perform the same tasks as the surgeon, only “several times faster and with more accuracy.”
New navigation technology also helps surgeons go beyond what their eyes can see, he says.
“If we put an MRI from before surgery into the computer system that commands the robot, we can see beyond the surface and eliminate human error. I can see better than my eyes, and the robot can move faster and work with more precision than my hands.” He and his team have been testing this approach in the lab for two years, and “already it helps surgeons by allowing them to operate sitting down.”
Advertisement
Not that this innovation will be his last.
“We want to take it further, to make the robot not just mechanical but a smart robot, a partner with the surgical team,” Dr. Kaouk says.
Advertisement
Advertisement

Honoring Exceptional Achievement, Service and Leadership

We celebrate the exceptional achievements of four future alumni

Honoring Exceptional Achievement and Leadership

Meet Hardeep Phull, MD (CCLCM’11)

Meet William Tierney, MD, MS (CCLCM’16, OTO’18)

Meet Samuel Omotoye, MD (CARD/E'15)