Is resection possible without major aortic bleeding?
An otherwise healthy man in his 60s presented to Cleveland Clinic with a complaint of back pain accompanied by chest discomfort. His history was remarkable for cervical spine surgery 10 years previously.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Chest imaging studies revealed a mass in the left mediastinum adjacent to the spine and touching the aorta (Figures 1 and 2). Biopsy confirmed diagnosis of a malignant paraspinal sarcoma, alternately referred to as a mediastinal sarcoma.
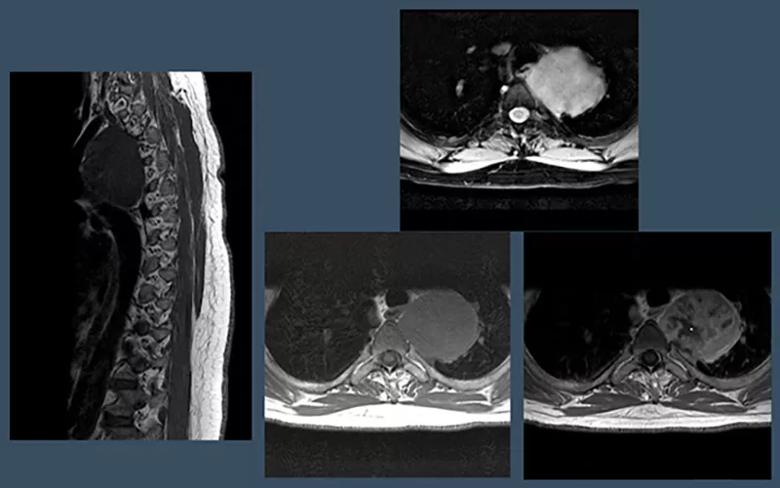
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ec15d740-a878-4bb3-9230-04cbec312f75/21-NEU-2275411-CQD-Inset-1-800x500-1_jpg)
Figure 1. Sagittal T1 MRI (left) and axial cuts of a thoracic MRI (T2 [top right] and T1 with and without gadolinium [bottom right]) at presentation showing a left-sided mediastinal/paraspinal mass abutting the lateral vertebral body and aorta.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dc81ea6c-e305-4843-84cc-efa8c8a9a0c6/21-NEU-2275411-CQD-Inset-2-800x435-1_jpg)
Figure 2. Coronal CT angiograms showing the left-sided mediastinal mass abutting the thoracic spine and aorta.
The patient was referred to Sudish Murthy, MD, PhD, Section Head of Thoracic Surgery, who consulted with Center for Spine Health neurosurgeon Ajit Krishnaney, MD.
Unless resected, sarcomas are associated with a relatively high mortality rate. High-dose radiation therapy is an option, but it carries far poorer outcomes. However, the unusual location of this sarcoma — nestled between spine and aorta — made resection daunting.
“In sarcoma cases, curative surgery requires resection of the tumor in one piece, with adequate margins to ensure removal of all malignant tissue,” notes Dr. Krishnaney. “Because the patient’s tumor touched the spine, it required removal of a margin of bone. Because it touched the aorta, obtaining an adequate margin there raised the prospect of major bleeding challenges.”
A subtotal resection followed by high-dose radiation was an option, but it still entailed a high enough risk of recurrence to prompt Drs. Murthy and Krishnaney to explore the feasibility of full resection.
Advertisement
The two surgeons had frequently collaborated in the past on cases of intrathoracic paraspinal masses, but this case involved an unprecedented complicating factor: the need for some degree of reconstruction of the aorta.
“If we couldn’t take a margin from the aorta, we wouldn’t be able to offer the chance of a cure,” Dr. Krishnaney explains. “There would be no point in undertaking the surgery.”
So they consulted with Eric Roselli, MD, Chief of Adult Cardiac Surgery and Director of Cleveland Clinic’s Aorta Center. After extensive discussion, the three surgeons collectively devised a plan for a three-stage operation involving a preparatory endovascular aorta surgery followed by a spine surgery and culminating in resection of the tumor with margins from both aorta and spine.
“We were reasonably confident this was resectable from the spine standpoint — the aorta was the question,” Dr. Krishnaney says. “When Dr. Roselli said he knew he could safely allow a margin to be taken from the outer surface of the aorta, that made everything possible.”
Treatment began with preoperative radiation therapy, overseen by radiation oncologist Chirag Shah, MD, of Cleveland Clinic Cancer Center, to enhance the likelihood of clean margins.
This was followed by the aorta procedure, in which Dr. Roselli placed a covered stent in the aorta spanning the area to be resected, thereby providing a channel for undisturbed blood flow after the outer wall of the aorta would later be peeled off with the tumor. “The use of an endovascular device to protect the aorta allowed for a staged procedure and less trauma to the patient,” Dr. Roselli explains. “It also obviated the need for high-dose heparin anticoagulation and cardiopulmonary bypass, which could have increased the risk of bleeding associated with the en bloc tumor resection.”
Advertisement
Five days later, the patient underwent the spinal portion of the operative plan. Using intraoperative navigation, Dr. Krishnaney performed an en bloc partial vertebrectomy with chest wall resection followed by spinal fusion and segmentation. “I used an osteotome to cut across the spine and ribs to free up tumor-involved bone from the chest wall, including part of the vertebral body, in order to loosen it and position it optimally for the subsequent resective thoracic surgery,” Dr. Krishnaney says. “We then placed screws and rods to restabilize the spine.”
Two days later, Dr. Murthy opened the chest from the side and resected the sarcoma en bloc (Figures 3 and 4), including margins from the spine and aorta. Dr. Roselli assisted in peeling the specimen from the outer wall of the aorta. There was no significant bleeding from the aorta, and its structure was maintained. In addition, the integrity of the spinal cord and supporting tissues was left intact (Figure 5). Final pathology confirmed a complete resection with negative margins.
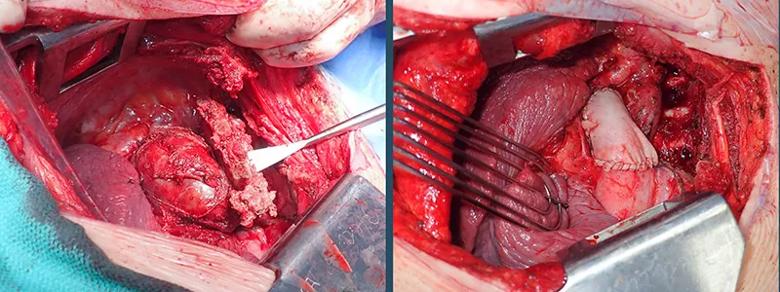
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f36bac59-25db-47e5-8888-f4c630bd7de4/21-NEU-2275411-CQD-Inset-3-800x300-1_jpg)
Figure 3. Photos of the surgical field before (left) and after (right) resection of the tumor and margins.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3767b624-9ed7-493e-b1d0-62d0d5fb24d4/21-NEU-2275411-CQD-Inset-4-800x575-1_jpg)
Figure 4. Photo of the resected tumor and margins.
The patient was discharged home within four days after the last operation and had an uneventful recovery. He has remained free of recurrence through one year of follow-up CT monitoring and has returned to an active lifestyle with no further complaints of back pain.
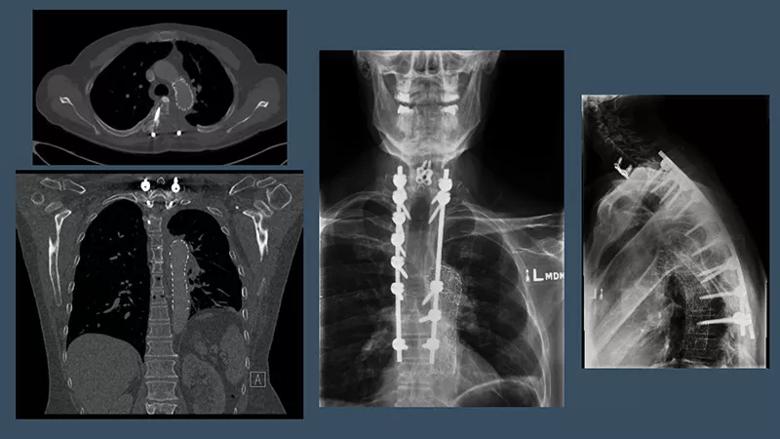
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/af8032eb-f7de-4c62-bb39-5dbb45906f45/21-NEU-2275411-CQD-Inset-5-800x450-1_jpg)
Figure 5. Postoperative axial and coronal CTs (left) and anteroposterior and lateral X-rays (right) showing complete resection of the mass and margins as well as spinal fixation hardware for spinal stabilization and the aortic stent in place.
Advertisement
This case marks the first paraspinal sarcoma resection at Cleveland Clinic involving reconstruction of the aorta, but Dr. Roselli notes that this technique has been used previously at Cleveland Clinic for intrathoracic malignancies from the lung infiltrating the aorta. Aortic resections for spinal tumors have been described previously in a limited number of case reports.
Beyond the operation’s novelty, it is notable for how it demanded three distinct surgical specialties working in concert to achieve success. The surgeons identify two factors essential to that success which should be considered by others undertaking similar cases.
1) An authentic culture of collaboration.All three surgeons cite the multidisciplinary culture promoted by Cleveland Clinic’s structure as critical to their ability to undertake this case. The surgeons were available on standby for each other as each undertook his respective portion of the three-part surgical plan.
“Collaboration across departments and institutes is easy and encouraged here, which is not always the case,” Dr. Krishnaney observes.
“This type of sophisticated multidisciplinary approach allows us to devise novel and innovative strategies to manage complex problems that cannot be treated similarly elsewhere,” adds Dr. Murthy.
2) A step-by-step strategy.Approaching the procedure in a staged fashion with meticulous planning was central to success. “Doing everything in one day might have been feasible but would have added an unnecessary level of complexity for both the patient and our teams,” says Dr. Krishnaney. “Our three-stage approach allowed us to fully concentrate on each component and make sure nothing was missed. Instead of enduring a 20-hour operation, each of us was able to complete our respective portions in under four or five hours. This helped reduce the risk to the patient and ensure we were all on our A-game.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches