Kits for use in healthcare settings can increase uptake
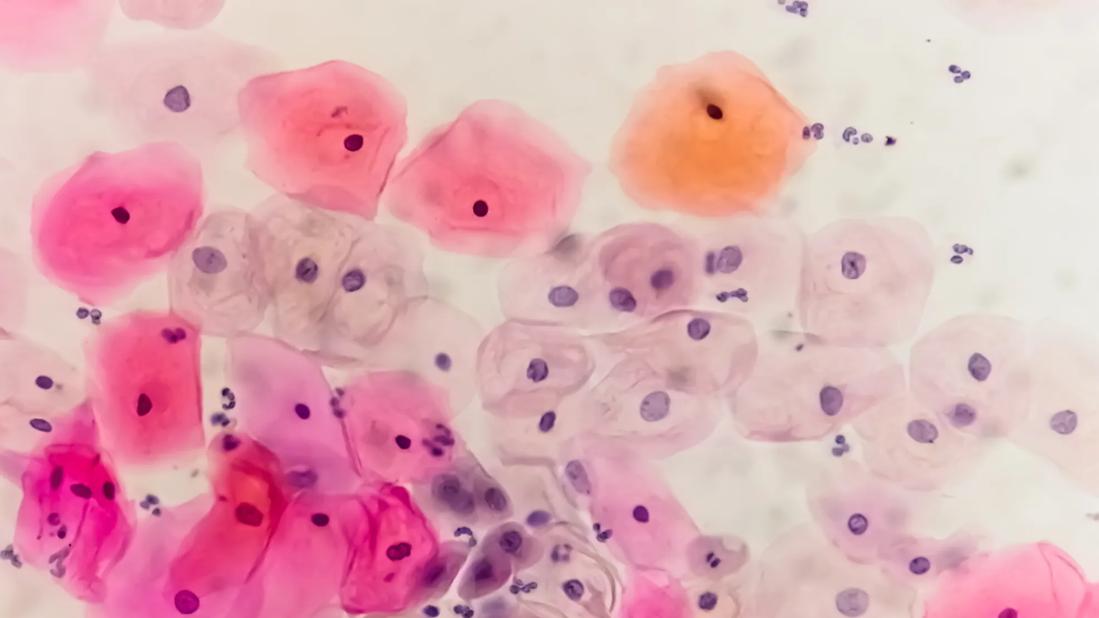
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c78f5efe-b2a6-4147-8716-4c911923914a/hpv-smear-1448826085)
cervical cancer cells
In 2024, the U.S. Food and Drug Administration approved two cervical cancer screening tests that allow women to collect their own vaginal specimens to detect human papilloma virus (HPV) — the cause of most cervical cancer. Now the U.S. Preventive Services Task Force is expected to update its guidance on cervical cancer screenings to include self-collected tests.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In Canada and some European countries, self-swab tests are approved for home use. The U.S. currently requires the tests to be done in a healthcare setting. Experts believe, however, that even allowing women to collect their own vaginal specimens in a healthcare setting is likely to increase screening uptake, thereby improving cancer detection and saving lives.
“Currently, almost 30% of women can’t or don’t get screened for cervical cancer at regular intervals,” says Cleveland Clinic radiation oncologist Sudha Amarnath, MD. She believes the self-administered screenings have the potential to do for cervical cancer what specimen self-collection has done for colorectal cancer screenings: provide some measure of protection for those who cannot or won’t have a colonoscopy.
When found early, cervical cancer is highly treatable and often curable. Historically, testing has been done by gynecologists or primary care physicians as part of routine pelvic examinations, using cervical cytology (Pap smear) or Pap plus an HPV test. Although deaths from cervical cancer in women under 25 have declined 65% since the introduction of HPV vaccines in 2006, significant risks remain. Only 54% of women in the U.S. have received all the recommended doses of the vaccine, and many women also are not regularly tested.
Reasons people give for not being screened vary, and they include patients not realizing they should be tested; geographic or financial barriers to healthcare; a history of sexual abuse or trauma; and finding the process embarrassing or unpleasant.
Advertisement
“The privacy piece is a big issue,” says Dr. Amarnath.” When it comes to pelvic exams, women do not always feel comfortable with their provider, or they might not always see consistent providers. So even being able to self-administer a test in a healthcare setting may make screening more accessible. That’s a huge benefit.”
In May 2024, the FDA approved self-collection for two tests that detect HPV strains known to cause cancer, calling the move “the latest example of the FDA’s continued commitment to expanding cervical cancer screening options for patients, particularly for individuals currently not participating/engaging in routine screening.”
Both work the same way, through insertion of a swabbing device that gathers cells from the vaginal wall. The tests are approved for women ages 30 to 65. (Women 21 through 29 should be tested every three years with cervical cytology. Women over 65 who were tested regularly and had no irregular results may be told they need not test any longer.)
“Healthcare settings” here includes the use of private areas or restrooms in primary care offices, urgent care centers, pharmacies and mobile clinics. “That expands access in a major way,” says Dr. Amarnath. “That can make a big difference, especially for people who don’t live close to a medical facility.”
Even among women with a history of being tested, scheduling regular exams can fall off as life becomes busier, she notes. “A lot of women we see haven’t had a Pap smear since their last child. Some stop going to doctors themselves because they’re taking care of everyone else. So being able to go to your local pharmacy and do this testing in the bathroom might be a little more accessible.”
Advertisement
The impact of more testing may have an even greater effect, she adds, if it creates an opportunity to encourage HPV vaccination for under-vaccinated individuals. The current HPV vaccine provides protection against nine strains known to cause cancers of the cervix, anus, and head and neck.
For some practitioners, patient self-testing may raise concerns. Cervical cancer screenings have long been considered part of regular pelvic examinations, which also include visual and physical examination of the reproductive organs and may include testing for sexually transmitted infections. Because self-administered tests cannot replace a pelvic exam, some physicians may feel uncomfortable prescribing them.
“It’s a big mind shift,” Dr. Amarnath acknowledges. “It’s similar to the way gastroenterologists felt about saying it’s OK to use colorectal cancer self-testing.”
Ultimately, however, the goal is to reach women who aren’t having pelvic exams in the first place. Prescribing the tests, and clearly communicating the need for follow-up care if results are positive or unclear, can have positive outcomes.
“We want to make sure people are getting screened, and also make sure they are getting in to see providers to follow up on any abnormal findings,” says Dr. Amarnath.
In the U.S., the Self-Collection for HPV Testing to Improve Cervical Cancer Prevention (SHIP) trial was begun in September 2024 to evaluate clinical accuracy of the self-collected tests versus clinician-collected samples. The research also will evaluate human factors that affect “usability, acceptability and preferences for self-collection.” SHIP is expected to be completed in October 2025.
Advertisement
“We have to make sure that when the test ends up in the hands of the people using it, it’s as effective as traditional methods,” says Dr. Amarnath. “It should be, but obviously nothing is perfect.”
Long range, she adds, the hope is that the self-collection tests will prove safe and effective so that the cervical cancer testing gap can be closed further.
“One of the biggest benefits down the road will be if this becomes available for home use.”
Advertisement
Advertisement
A new analysis emphasizes the value of a multi-disciplinary approach.
Studying trends of conization with lymph node evaluation, trachelectomy and radical hysterectomy
Multidisciplinary teams work together in in-situ scenarios
Uterine transposition cleared the field for radiation therapy
ACOG-informed guidance considers mothers and babies
Prolapse surgery need not automatically mean hysterectomy
Artesunate ointment shows promise as a non-surgical alternative
New guidelines update recommendations