Molecular study suggests an update to AJCC guidelines
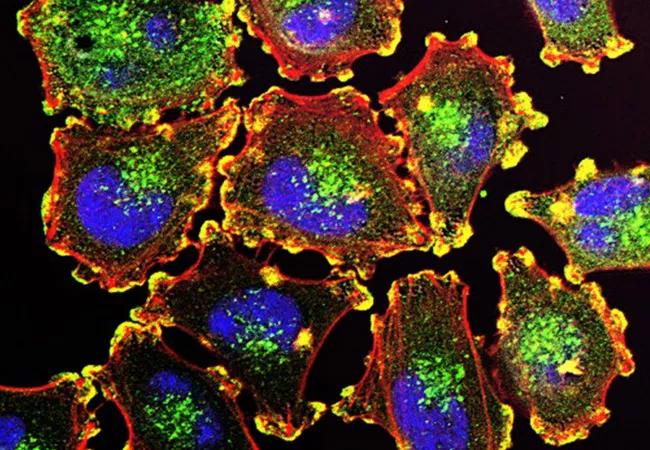
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a6e31f9f-01ab-41dc-a35e-c001e5f3ecc9/nci-vol-9872-72_650x450_jpg)
Metastatic melanoma cells. Image source: National Cancer Institute
The molecular characteristics of melanomas of the female genital tract fit more closely with those of mucosal than those of cutaneous melanoma, according to a recent review of 37 cases led by Shabnam Zarei, MD, Cleveland Clinic pathologist. Current American Joint Committee on Cancer (AJCC) staging guidelines recommend grouping vulvar melanoma with cutaneous melanoma and provide no guidance on staging vaginal melanoma. Dr. Zarei and colleagues’ findings suggest a change in current clinical practices and future guideline development.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Historically, we have focused on anatomic distribution alone to fit melanoma into different staging categories — vulvar or vaginal, cutaneous or mucosal,” says Chad Michener, MD, Interim Chair of Cleveland Clinic’s Department of Subspecialty Care for Women’s Health. “Dr. Zarei’s work questions that focus and shifts it to a genomic basis.”
The seventh iteration of the AJCC recommendations for staging vaginal melanomas aligned with Dr. Zarei’s findings. However, in the eighth release, that guideline was removed entirely. “The guidelines changed because we have no staging system that seems to be highly predictive of prognosis, especially in vaginal melanoma, not FIGO [International Federation of Gynecology and Obstetrics] or Clark’s staging or tumor thickness or Breslow’s depth. The data we have favor using the cutaneous melanoma TNM staging system for vulvar melanoma,” says Dr. Michener. “That’s why Dr. Zarei’s data is exciting.”
The study, published in the International Journal of Gynecological Pathology, evaluated the mutational status of 37 vulvar, vaginal and urethral melanoma patients with clear notation of primary tumor site (vulvar dermal, vulvar mucosal, vaginal and urethral) in their medical records. Thirty percent of patients had tumors of the hair-bearing vulva, 22% from the vagina, 19% from the urethra, 16% from vulvar glabrous skin, 8% from the junction of vulvar dermal and vulvar mucosal tissue and 5% from rectal and rectovaginal mucosa.
The research team used a DNA-targeted next-generation sequencing (NGS) panel analyzing the most common genetic mutations in melanomas to evaluate the cases. The panel provided whole exome coverage of 9 genes and mutational hotspot coverage in another 12 genes, and results were classified as pathogenic, likely pathogenic or variant of unknown significance.
Advertisement
Results showed that the three most common genetic alterations were KIT (32%), TP53 (22%) and NFI (19%). Two-thirds of cases had a pathogenic alteration in one or more of the MAPK pathway genes. Notably, none of the differences among mutation profiles in the primary tumor site groups were statistically significant, and overall survival rates were similar among groups.
“We were able to show that melanomas from different sites in the lower genital tract have similar molecular signatures as well as similar overall survival rates,” says Dr. Zarei. “Thus, we believe that vulvar and vaginal melanomas can be grouped together for staging purposes using AJCC mucosal melanoma guidelines.”
Dr. Zarei’s work challenges existing guidelines for staging melanomas of the lower genital tract and suggests a change in practice is necessary. “These are rare cancers, and we don’t understand enough about their biology to accurately predict outcomes. Our study offers evidence that suggests we need to think about these diseases differently,” says Dr. Zarei.
But the data aren’t there quite yet. “While further studies are needed to show that the mucosal melanoma staging system predicts outcomes for vulvar and vaginal melanomas,” adds Dr. Michener, “Dr. Zarei’s work is an exciting step forward in the use of molecular and genomic data to identify more accurate prognostic indicators in vulvar and vaginal melanomas.”
Image: Metastatic melanoma cells. Image source: National Cancer Institute
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches