Teaching students without compromising patient safety

In a recent article published in the American Journal of Obstetrics & Gynecology, the Association of Professors of Gynecology and Obstetrics Undergraduate Medical Education Committee (UMEC) provided an overview of the use of simulation in medical education. Consult QD sat down with Margaret McKenzie, MD, President of Cleveland Clinic South Pointe Hospital, UMEC member and co-author of the paper, to discuss how she uses simulation with her medical students.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The former teaching method involved student participation in patient care. This is decreasing in popularity for a number of reasons. The increasing demand and burnout in our profession are well publicized. Preceptors have less time to teach, but simulation is gaining popularity for other reasons as well.
Medical students previously spent a lot of time observing. However, many times in Ob/Gyn practice, women prefer to maintain their privacy, and I don’t blame them… but medical students don’t learn much by waiting outside the exam room. We’ve found that using simulated scenarios allows students to practice clinical tasks and communication skills, developing the knowledge and behaviors they need without sacrificing patient comfort.
Additionally, simulation in medical education has been brought about by changes in healthcare and increasing concerns for quality and patient safety. We learn by practicing until we master a skill, and mistakes are a significant component of the learning process. With simulation, students are able to practice skills—from suturing to pelvic exams—until they achieve mastery without harm to patients.
A student would never have the opportunity to place an IUD in most settings… But you want a student to understand the principles, the anatomy and so forth. For example, a papaya can be used to simulate a uterus as students learn to insert IUDs.
We also use simulation to teach a mixture of technical and interpersonal skills, including breast exams, pelvic exams with Papanicolaou smear collection, labor cervical exams, endometrial biopsies and hysteroscopy. For some simulations, such as hysteroscopy, we use computerized virtual reality. The system we have looks just like a video game, which in fact mimics the experience of performing hysteroscopy in real life.
Advertisement
Students tend to get really excited because they like “doing” things. This results in more engagement and interaction with professors. Simulated learning environments can also facilitate effective feedback and assessment. I think it gives both students and teachers time to bond without a lot of pressure, and not having all that pressure allows for practice and encourages patience.
As a student, it can take a while to locate the cervix. The patient is already uncomfortable, and prolonged internal evaluations in the middle of labor can make this worse. Students may feel increased pressure to conduct the exam quickly. Instead, we use low-fidelity props or mannequins to ensure students understand the labor and delivery process, including cervical changes. We encourage exploration using a mannequin. The first time students perform a labor cervical examination, I instruct them to just get their fingers in the [simulated] vagina and get comfortable. The next time, they might try to locate the cervix, and so on…
It works really well when you use actors, or what we call standardized patients. You can train the standardized patient to act like a real patient and help students develop an appreciation of the patient and caregiver experiences. We use checklists and give instant feedback in a non-threatening environment. We train our standardized patients really well so they look and act like patients, but they also help manage the students throughout the simulation.
Our goal, as educators, is to create a safe space where learners thrive—a space where everyone feels safe saying what they know and they don’t know. Through simulation, students and professors work together in a non-judgmental environment. This creates a culture of of feedback, and reflection on feedback, allowing students to figure out what gaps they need to fill.
Advertisement
The UMEC group found evidence to support the expanded use of simulation in Ob/Gyn medical student training. Simulation-based medical education fosters a learning environment in which students have the opportunity to practice the clinical, communication and leadership skills necessary to provide quality patient care.
Advertisement
Advertisement

Advanced software streamlines charting, supports deeper patient connections

How holding simulations in clinical settings can improve workflow and identify latent operational threats

Interactive Zen Quest experience helps promote relaxing behaviors

Cleveland Clinic and IBM leaders share insights, concerns, optimism about impacts
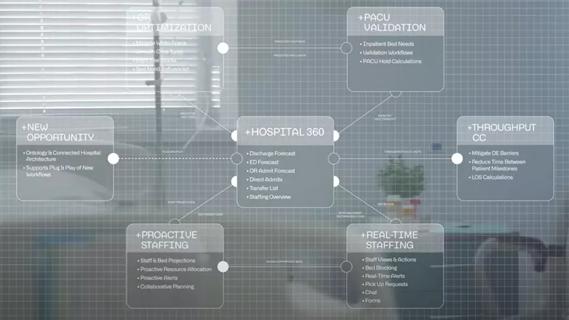
Cleveland Clinic partners with Palantir to create logistical command center

A Q&A with organizational development researcher Gina Thoebes

Cleveland Clinic transformation leader led development of benchmarking tool with NAHQ

Raed Dweik, MD, on change management and the importance of communication